Regenerative Medicine News and General Information
An Innovative Technology Has Been Developed to Enable Bone Regeneration
Reconstruction of bone defects that cannot heal spontaneously, that is, critical-sized bone defects, continues to be an enormous clinical challenge. Such defects may result from trauma, inflammation or following bone tumor resections. Although autogenic, allogeneic and xenogeneic bone materials have been widely applied to treat such defects, they possess potential limitations, including limited availability and donor site morbidity , potential immunogenicity and risk for disease transmission.
The classic tissue engineering approach, involving the use of living cells, growth factors and a basic scaffold, has emerged as a promising tool to address these issues. However, despite the undoubted potential held by this approach, it still involves ex vivo cell manipulation, which may have immunogenic and tumorigenic potential.
Hydrogels are of particular interest as cell-ingrowth scaffolds for tissue engineering and bone regeneration, as they offer a three-dimensional (3D) network for cell attachment and growth. Specifically, naturally occurring polysaccharides, including hyaluronic acid (HA), alginate (Alg) and chitosan, have elicited an immense amount of attention due to their high biocompatibility, biodegradability, low immunogenicity and abundance in nature. Nevertheless, their usefulness has been limited by unsatisfactory mechanical properties and a high degradation rate.
An alternative method to strengthen polysaccharides is by integrating them with self-assembling short peptide hydrogelators to create composite hydrogels with improved and tunable mechanical properties.
An innovative technology has been developed to enable bone regeneration
The groundbreaking study was conducted by experts from TAU’s Maurice and Gabriela Goldschleger School of Dental Medicine, led by Prof. Lihi Adler-Abramovich and Dr. Michal Halperin-Sternfeld, in collaboration with Prof. Itzhak Binderman, Dr. Rachel Sarig, Dr. Moran Aviv, and researchers from the University of Michigan in Ann Arbor.
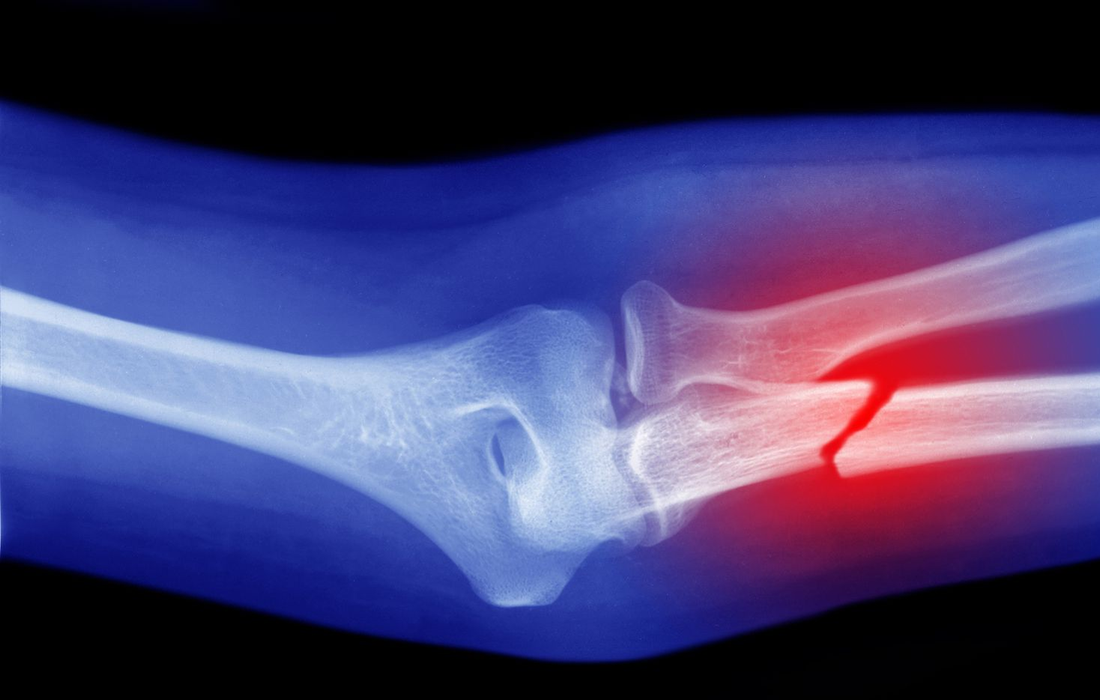
Small bone defects, such as fractures, heal spontaneously, with the body restoring the lost bone tissue. The problem begins with large bone defects. In many cases, when substantial bone loss results from tumor resection (removal by surgery) , physical trauma, tooth extraction, gum disease or inflammation around dental implants, the bone is unable to renew itself.
In the current study, they developed a hydrogel that mimics the natural substances in the extracellular matrix of bones, stimulating bone growth and reactivating the immune system to accelerate the healing process .
The researchers explain that the extracellular matrix is the substance surrounding our cells, providing them with structural support. Every type of tissue in our body has a specific extracellular matrix consisting of suitable substances with the right mechanical properties. The new hydrogel has a fibrillary structure that mimics that of the extracellular matrix of the natural bone. Furthermore, it is rigid, thus enabling the patient’s cells to differentiate into bone-forming cells.
In the study, they produced a hydrogel that mimics this specific matrix in both chemical and physical properties. At the nanometric level, the cell can attach itself to the gel, gaining structural support and receiving relevant mechanical signals from the fibers. At first, to test these properties, they grew cells in a 3D model of the gel. Then they examined the impact of the hydrogel on model animals with large bone defects that could not heal spontaneously. They monitored them for two months with various methods, including Micro C.T. To our delight, the bone defects were fully corrected through regeneration, with the bones regaining their original thickness, and generating new blood vessels.
The hydrogel served as a 3D matrix that maintained the space over time and was then gradually degraded while promoting the host’s natural bone healing process by modulating the local immune environment in favor of angiogenesis, osteogenesis and the osteointegration of the implanted hydrogel. Finally its simple production, relatively low cost and ease of handling and delivery, demonstrate its potential for use in various clinical applications in bone regenerative medicine.
SOURCE:
Michal Halperin‐Sternfeld, Ariel Pokhojaev, Moumita Ghosh, Dana Rachmiel, Raha Kannan, Itzhak Grinberg, Moshe Asher, Moran Aviv, Peter X. Ma, Itzhak Binderman, Rachel Sarig, Lihi Adler‐Abramovich (September 15, 2022). Immunomodulatory fibrous hyaluronic acid‐ Fmoc ‐diphenylalanine‐based hydrogel induces bone regeneration. Journal of Clinical Periodontology. Retrieved from : https://onlinelibrary.wiley.com/doi/10.1111/jcpe.13725