Stem Cell Therapy for Specific Conditions
Is More Mesenchymal Stem Cells Better? New Study Results
Mesenchymal stem cells (MSCs) have gained great interest as new medical treatments for multiple medical conditions. MSCs act by three major classes of mechanisms:
- Differentiation into specific types of cell lineages and integration into tissues.
- Secretion of factors including cytokines and exosomes that promote cell survival and growth, and that modulate inflammation.
- Direct MSC contact with host cells to modulate functions of effector cells.
The first and most widely used source of MSCs in clinical trials is bone marrow (BM). MSCs are isolated by adherence to plastic dishes, and are capable of differentiating into osteocytes, chondrocytes, and adipocytes, express proteins such as CD105, CD73, and CD9, and lack CD45, CD34, CD14, CD9, and HLA class II.
After BM, adipose tissue and umbilical cord (UC) are the most common sources and account for the majority of clinical trials. Different factors make comparisons between different clinical trials difficult, including heterogeneity among MSCs from different sources, use of different cell preparation protocols, and different doses of MSCs.
New Study Results
In a study published in the journal Stem Cells Translational Medicine, researchers conducted a study to generate a current database of clinical trials and results reported, and to analyze the routes of administration and doses for MSCs.
The research team extracted information from 914 trials that included multiple routes of MSCs administration, including intravenous, intraarterial, intrathecal, intraarticular and intracardiac, and also included different doses.
BM aspirates from the pelvis has been and continues to be the most frequently used source of MSC for clinical trials, with umbilical cord being the second most common source of MSCs used in clinical trials with their numbers being modestly higher than trials using MSCs derived from adult adipose tissue by liposuction.
The intravenous administration route has the highest average MSCs dose, and is also the most prevalent in general and for disorders including neurological, pulmonary, inflammatory bowel disease, liver, skin, diabetes, and kidney problems. Other routes of delivery most frequently matched their tissue targets, for example, IAT for joint, IC for cardiovascular, and IM for muscle.
The team selected individual trials that reported efficacy for multiple doses of the same cells, to do a direct comparison of doses without variability in cells and protocols used, which included 28 trials, all reporting safety, including nine phase 1 trials.
In a trial for type 2 diabetes single blind trial, three doses were tested and only the highest dose of 140 million cells/patient yielded significant reduction in the clinical target HbA1c. Another trial evaluating MSCs for diabetic nephropathy, which was a double blind trial, a dose of 150 million, significantly improved estimated glomerular filtration rate at week 12 within a subgroup.
Of the total studies included in the research, the combined results suggest a minimal effective dose (MED) range between 100 and 150 million cells, whereas doses of 70 million or lower and doses of 200 million or higher were less or not effective.
The team found that of the trials included in the study the effective IV doses ranged from 70 to 190 million cells/patient/dose suggesting many MSCs act with comparable efficacy by common mechanisms involving factor secretion and contact-mediated immune cell modulation in many different inflammatory conditions.
Some studies showed a therapeutic response at doses of 140 and 150 million cells/patient/dose for patients with Crohn’s disease. However, another trial using a dose of 750 million/patient/dose was not effective suggesting that it might be too high. The researchers believe that this could be due to an excessive immune modulation.
The appropriate dose and minimal effective dose remains to be studied with further studies, but with the current research information it appears that higher doses than 150 million per treatment may not be necessary, and that more is not necessarily always better.
Stem Cell Therapy at Zignagenix
At our clinic we offer different therapeutic procedures. We always recommend intravenous therapy for all of our patients in combination with localized injections depending on the patient’s condition. We have a variety of MSCs packages starting at 30 million and going up to 200 million stem cells, which falls into the range that this study and others have shown good therapeutic results for multiple health conditions.
Sources:
Kabat M, Bobkov I, Kumar S, Grumet M. Trends in mesenchymal stem cell clinical trials 2004-2018: Is efficacy optimal in a narrow dose range?. Stem Cells Transl Med. 2020;9(1):17-27. doi:10.1002/sctm.19-0202
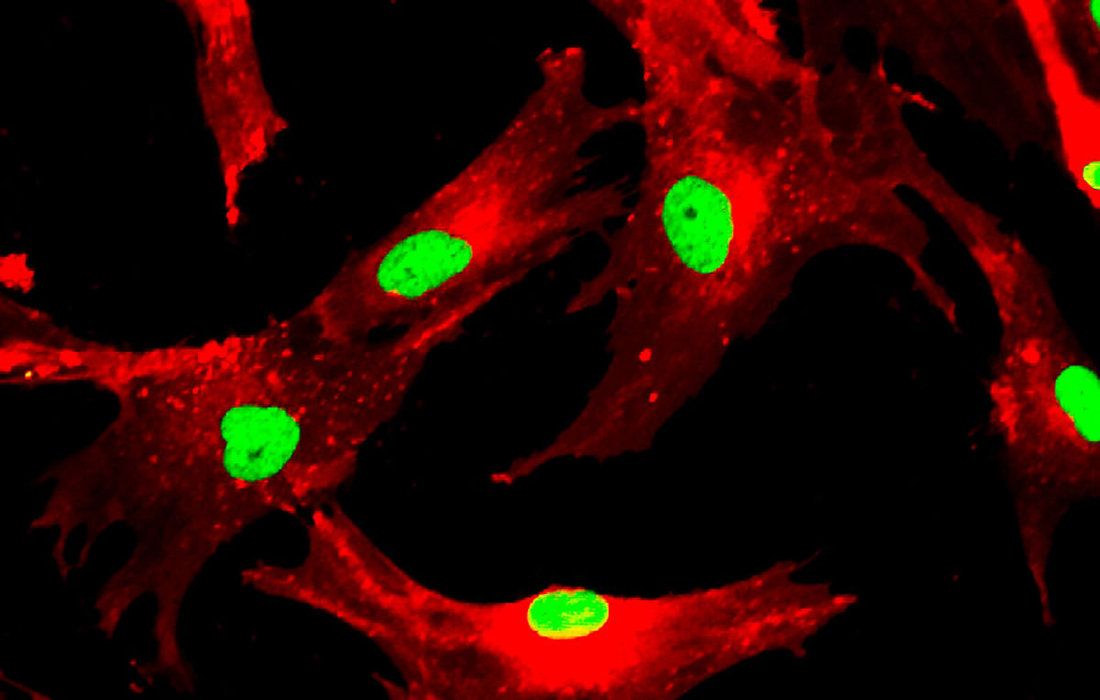
Image from: