Stem Cell Therapy for Specific Conditions
MSCs Treatment in Severe Pulmonary Arterial Hypertension
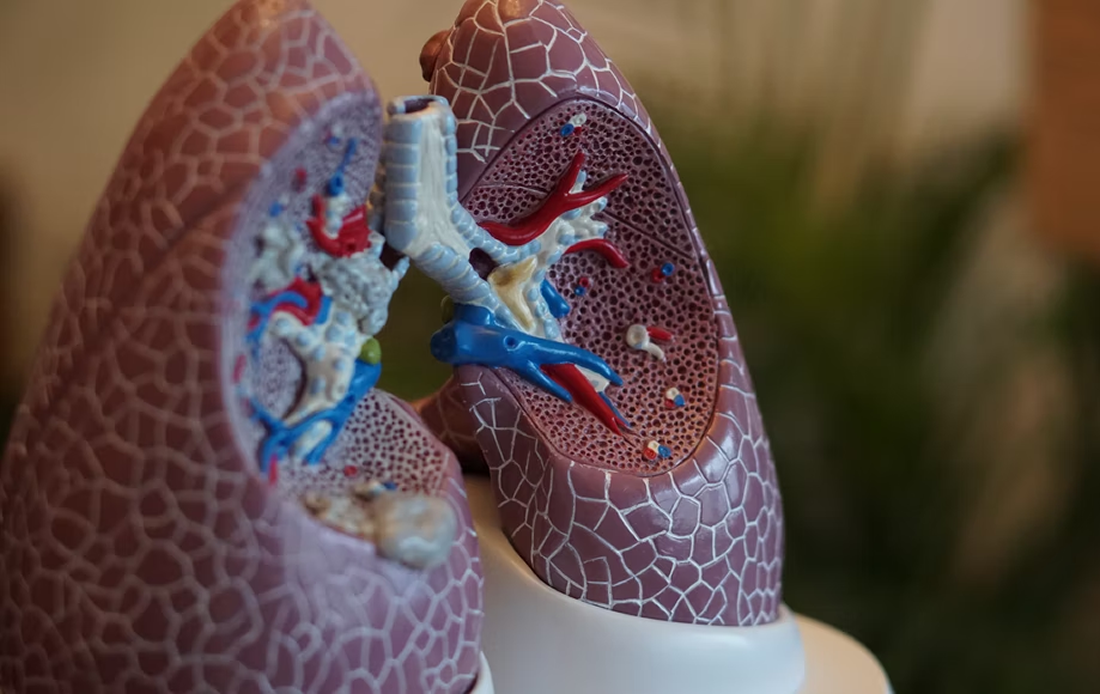
What is Pulmonary Arterial Hypertension?
Pulmonary Arterial Hypertension (PAH) is characterized by progressive, obliterative remodeling of pulmonary arterioles, pre-capillary vessel loss, right heart failure and death.
The pathobiology of pulmonary vascular disease (PVD) and PAH is complex, multifactorial and driven by inflammation and metabolic dysfunction.
Despite improvements in pharmacotherapy for PAH, advanced PAH is still a non-curable condition.
Use of MSCs and Regenerative Therapies
The use of mesenchymal stem cells is considered a potential therapy for their capability of secreting multiple growth factors and cytokines that can regulate the immune response and decrease inflammation.
Recently a group of researchers published a case report of a 3 year-old female that presented with heritable PAH associated with hereditary hemorrhagic telangiectasia. The results of the study appear in the journal Nature Cardiovascular Research.
The 3-year old patient had a history of afebrile seizure episodes, a 6 minute walking distance of only 270 meters and moderate thrombocytopenia. She also had a 10-month history of fatigue, repetitive nosebleeds and mucocutaneous telangiectasia at the lips, chest and lower extremities.
She also presented severely compromised right ventricular function with tricuspid regurgitation. The patient was on dual oral combination therapy with sildenafil, macitentan, spironolactone and inhalative iloprost and referred for a lung transplant evaluation.
Human umbilical cord mesenchymal stem cells (HUCMSCs) from the patient’s younger sibling’s umbilical cord were isolated.
The patient received five HUCMSCs infusions over 6 months during 2 hospital stays via an intrapulmonary arterial catheter and a central venous catheter. All infusions were well tolerated.
Improved Symptoms and Decreased Inflammation Levels
In the interval between diagnosis and the start of the therapy the patient essentially had no weight gain and no growth in 12 months. After the therapy was initiated the patient started to grow +10 cm in length in 3 months, her cardiopulmonary exercise capacity greatly increased, increasing her 6 meter walking distance to 485 meters.
HUCMSC-derived therapy decreased patient blood plasma markers of vascular (endothelial) fibrosis (NEDD9), vascular injury (ICAM-1) and inflammation (SAA; IFN-γ).
Overall, the treatment markedly improved her clinical and hemodynamic parameters and decreased her blood plasma levels of vascular fibrosis, injury and inflammation.
According to the researchers, the girl is now 6 years old and doing very well, without any limitations in exercise capacity.
Source:
Hansmann, G., Chouvarine, P., Diekmann, F. et al. Human umbilical cord mesenchymal stem cell-derived treatment of severe pulmonary arterial hypertension. Nat Cardiovasc Res 1, 568–576 (2022). https://doi.org/10.1038/s44161-022-00083-z
Image from:
Photo by Robina Weermeijer on Unsplash