Regenerative Medicine News and General Information
New Antitumor Cells to Treat Blood Diseases and Cancer Tumors: Study
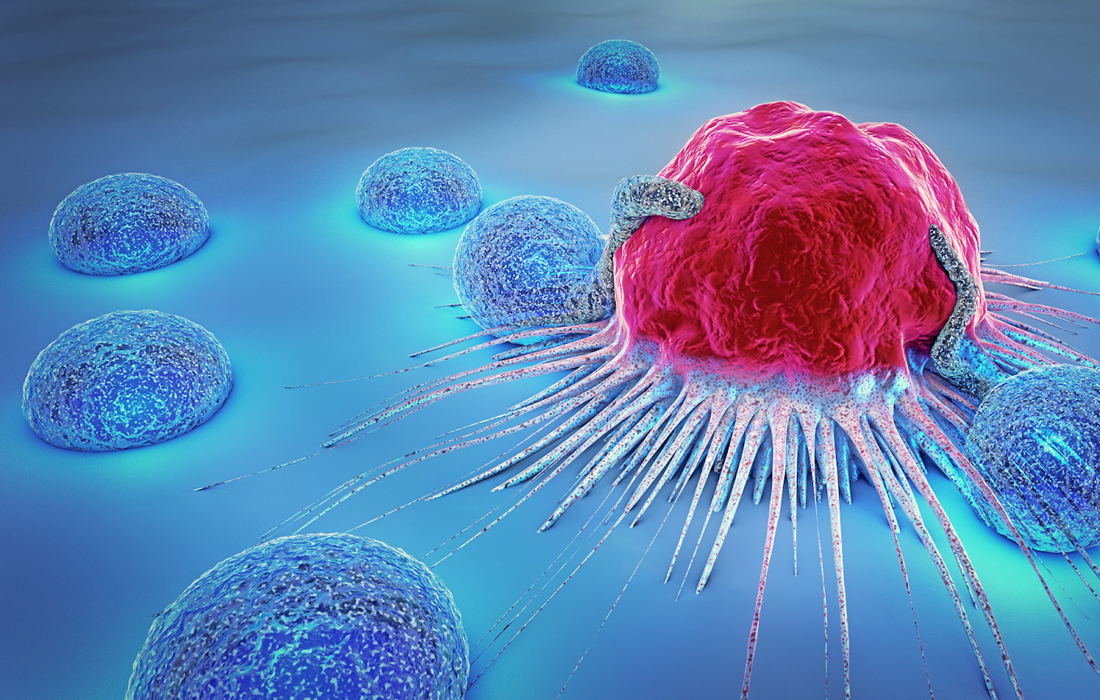
Neutrophils, the most abundant circulating leukocytes in humans, accumulate in many types of tumors and represent a significant portion of tumor-infiltrating cells.
Due to their heterogeneity and plasticity in the tumor microenvironment (TME), neutrophils have demonstrated contradictory protumor and antitumor effects during tumor evolution.
For instance, tumor-associated neutrophils present direct or antibody-dependent cytotoxicity against solid tumors , whereas they also facilitate angiogenesis, promote tumor metastasis, and suppress antitumor function of other cells in the TME.
Protumor neutrophils also reduce the efficacy of cancer therapies , including immunotherapies, leading to the development of neutrophil-targeted strategies for treating various cancers.
However, given the high heterogeneity of neutrophils in the TME, general suppression via small molecules or antibodies may eliminate both protumor and antitumor neutrophils and decrease the efficacy of neutrophil-targeted therapy.
Modified Neutrophils and Human Stem-Cells against Tumors
Xiaoping Bao, a Purdue University assistant professor from the Davidson School of Chemical Engineering, said CAR-neutrophils, or chimeric antigen receptor neutrophils, and engraftable HSCs, or hematopoietic stem cells, are effective types of therapies for blood diseases and cancer. Neutrophils are the most abundant white cell blood type and effectively cross physiological barriers to infiltrate solid tumors. HSCs are specific progenitor cells that will replenish all blood lineages, including neutrophils, throughout life.
Bao has developed a patent-pending method to mass-produce CAR-neutrophils from human pluripotent stem cells (hPSCs), that is, cells that self-renew and are able to become any type of human cell.
The chimeric antigen receptor constructs were engineered to express on the surface of the hPSCs, which were directed into functional CAR-neutrophils through a novel, chemically defined protocol. These hPSC-derived neutrophils displayed superior and specific antitumor activities against glioblastoma after engineering with chimeric antigen receptors.
In summary, the CAR-neutrophil engineering platform described here may serve as a scalable strategy to make available neutrophils as standardized cellular products for clinical applications in cancer and neutropenia treatment. Given the relative ease of gene editing in hPSCs, other genetic modifications, such as multiple CAR expressions, can also be performed to achieve optimal therapeutic effects in CAR neutrophils.
Due to their native ability to cross the blood-brain-barrier and penetrate brain parenchyma, neutrophil-mediated delivery of therapeutic drugs into brain has improved glioblastoma diagnosis and treatment , and such a combination may further enhance antitumor activities of hPSC-derived CAR neutrophils. Importantly, stable CAR-expressing hPSC lines can be also used to produce off-the-shelf CAR T and NK cells.
These cells are not readily available for broad clinical or research use because of the difficulty to expand ex vivo to a sufficient number required for infusion after isolation from donors
SOURCE:
Yun Chang, Ramizah Syahirah, Xuepeng Wang, Gyuhyung Jin, Sandra Torregrosa-Allen, Bennett D. Elzey, Sydney N. Hummel, Tianqi Wang, Can Li, Xiaojun Lian, Qing Deng, Hal E. Broxmeyer, Xiaoping Bao, (July 19, 2022). Engineering chimeric antigen receptor neutrophils from human pluripotent stem cells for targeted cancer immunotherapy. Cell Reports. Retrieved from:
IMAGE:
https://www.datasci.com/images/default-source/default-album/cancer-cell.jpg?sfvrsn=2dd9ee65_0