Regenerative Medicine News and General Information
New Promise Mechanism to Generate Cartilage Cells
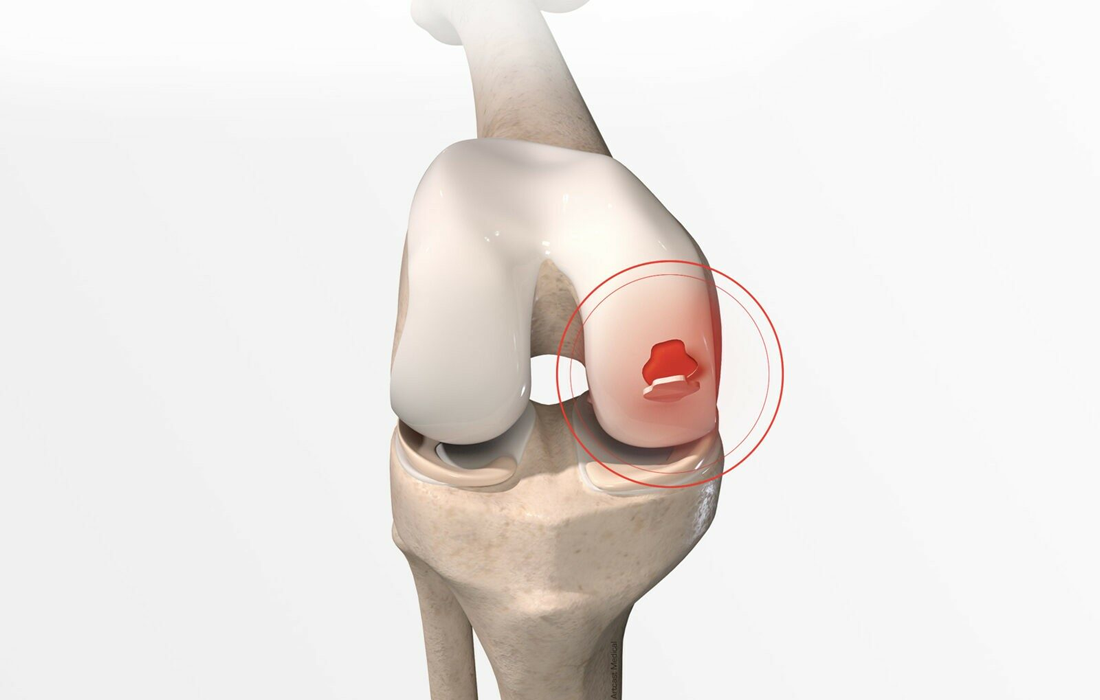
Cartilage degeneration and injuries affect 350 million people worldwide. Patients with these conditions experience increased pain and discomfort over time. However, an exciting breakthrough in tissue regeneration research offers the promise of meaningful relief. The study, led by faculty at The Forsyth Institute, suggests a new approach for making cartilage cells with huge implications in regenerative medicine for future cartilage injuries and degeneration treatments.
As any weekend warrior understands, cartilage injuries to joints such as knees, shoulders, and hips can prove extremely painful and debilitating. In addition, conditions that cause cartilage degeneration, like arthritis and temporomandibular joint disorder (TMJ), affect 350 million people in the world and cost the US public health system more than $303 billion every year. Patients suffering from these conditions experience increased pain and discomfort over time.
However, an exciting study led by faculty at The Forsyth Institute suggests new strategies for making cartilage cells with huge implications in regenerative medicine for future cartilage injuries and degeneration treatments. In a paper, entitled “GATA3 mediates nonclassical β-catenin signaling in skeletal cell fate determination and ectopic chondrogenesis,” co-first authors Takamitsu Maruyama and Daigaku Hasegawa, and senior author Wei Hsu, describe two breakthrough discoveries, including a new understanding of a multifaceted protein called β-catenin.
Dr. Hsu is a senior scientist at the Forsyth Institute and a Professor of Developmental Biology at Harvard University. He is also an affiliate faculty member of the Harvard Stem Cell Institute. Other members conducting the study included Swiss scientists Tomas Valenta and Konrad Basler, and Canadian scientists Jody Haigh and Maxime Bouchard. The study appears in the most recent issue of Science Advances.
“The goal of this study,” said Dr. Maruyama of Forsyth, “was to figure out how to regenerate cartilage. We wanted to determine how to control cell fate, to cause the somatic cell to become cartilage instead of bone.”
Previously, it was thought that the Wnt signal transduction pathway was the determinant of whether a cell became bone or cartilage. The master factor transducing the Wnt signals is β-catenin. The basis for this belief was the result that when β-catenin was disrupted, the bone became cartilage.
However, β-catenin also acts as a cell adhesion molecule to facilitate cell-cell interaction — the original function identified prior to the discovery of its role in Wnt signaling. “We know that this molecule is important for cell fate determination, but the mechanism remains open to study,” said Dr. Hsu.
The team tested what would happen when β-catenin was only partially impaired for signaling, finding that, in that case, the cells were unable to form bone or cartilage. After these tests, the scientists concluded that Wnt signaling is a determinant for bone formation, but that it isn’t sufficient for cartilage generation.
“We wanted to know what the factor was for cell fate determination,” said Dr. Maruyama. “What reprograms a cell to become cartilage if it isn’t Wnt signaling?”
This question led to a second major discovery: GATA 3, an alternative action of β-catenin responsible for skeletal cell fate switching. GATA3 is a single gene regulator, which turns on cartilage-specific gene expression in cells. “Basically,” said Dr. Wei Hsu, “GATA3 binds to the genome sequences required for the reprogramming. GATA3 is a game changer because we can use it to potentially change any somatic cell to become a cartilage-forming cell, similar to using four stem cell factors to generate embryonic stem cell-like cells called induced pluripotent stem cells (iPSC).”
Being able to control the cell’s fate in this way makes it possible to direct a cell to become bone, cartilage, or fat, which has tremendous implications for creating new treatments for the 1 in 4 people living with cartilage injuries and cartilage degeneration. There is currently no treatment that can regenerate cartilage, and current treatments are unable to improve joint function.
This research opens new avenues for scientists to explore and is an exciting breakthrough in tissue regeneration research with the promise of meaningful relief for thousands of patients.
SOURCE:
Forsyth Institute. (2022, November 30). Scientists discover a new mechanism to generate cartilage cells. ScienceDaily. Retrieved December 8, 2022 from www.sciencedaily.com/releases/2022/11/221130151516.htm
IMAGE: