Regenerative Medicine News and General Information
One Type of Gut Bacteria May Contribute to the Development of Type 2 Diabetes
In recent decades, the prevalence of type 2 diabetes has increased dramatically. We refer to insulin sensitivity, insulin secretion, and insulin clearance as components of “insulin homeostasis,” given that these traits encompass action, production, and removal of insulin. Dysfunction in insulin sensitivity and insulin secretion underlie the development of type 2 diabetes. The role of insulin clearance is less well established . Insulin clearance may contribute to diabetes pathogenesis in high-risk populations. A major goal of diabetes research is to determine mechanisms whereby insulin homeostasis deteriorates and predisposes to diabetes.
Studies have implicated genetic factors, unhealthy diet, insufficient physical activity, suboptimal sleep, and obesogenic environmental factors. A recent addition is dysbiosis of the gut microbiome.
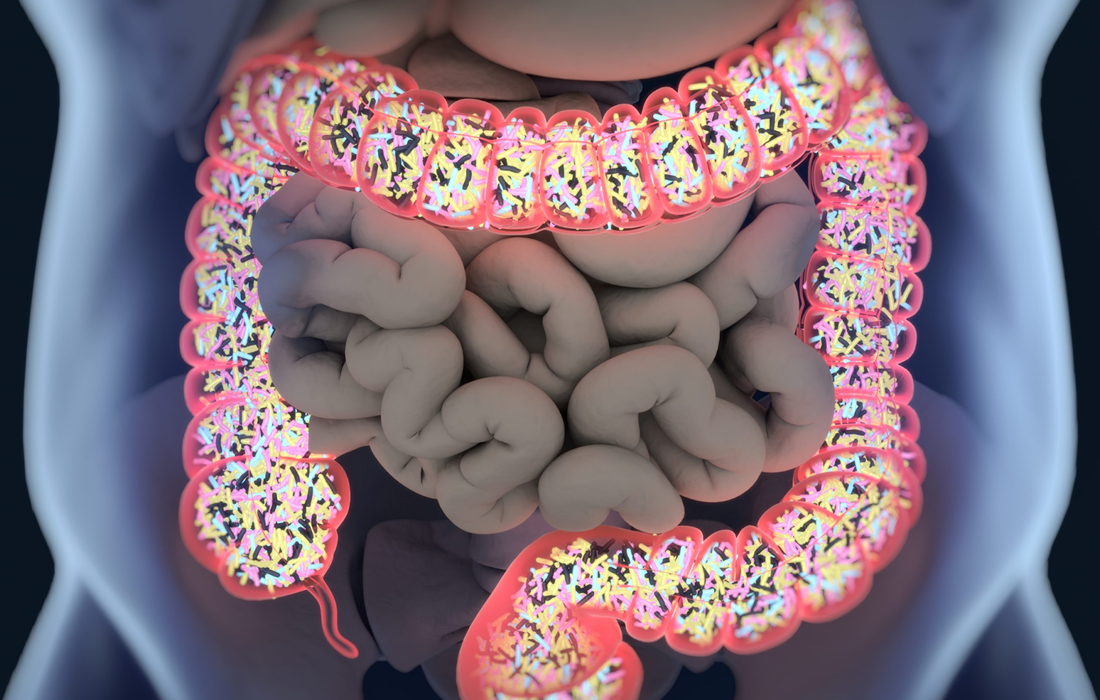
The gut microbiota consists of a diverse community of bacteria. Although relatively stable in adults, the gut microbiome can be altered by diet and medications. High-throughput sequencing technology has facilitated large-scale microbiome profiling in individuals with prediabetes or diabetes versus controls, as recently reviewed. A recurrent finding in these studies was depletion of bacterial species that produce short-chain fatty acids (SFCAs), particularly butyrate, in individuals with type 2 diabetes.
Butyrate, propionate, and acetate are the most abundant SCFAs in the human gastrointestinal tract. Intestinal microbes generate SCFAs by fermenting dietary carbohydrates that humans cannot digest. SCFAs have been extensively reported to improve glucose homeostasis and metabolism in adipose, muscle, and liver tissues.
The relationships between butyrate-producing bacteria and distinct metrics of insulin homeostasis have not been thoroughly explored, and prior human studies.
A study found people with higher levels of a bacterium called Coprococcus tended to have higher insulin sensitivity, while those whose microbiomes had higher levels of the bacterium Flavonifractor tended to have lower insulin sensitivity
Mark Goodarzi, MD, PhD, the director of the Endocrine Genetics Laboratory at Cedars-Sinai, is leading an ongoing study that is following and observing people at risk for diabetes to learn whether those with lower levels of these bacteria develop the disease.
investigators analyzed data from 352 people without known diabetes who were recruited from the Wake Forest Baptist Health System in Winston-Salem, North Carolina.
Study participants were asked to attend three clinic visits and collect stool samples prior to the visits. Investigators analyzed data collected at the first visit. They conducted genetic sequencing on the stool samples, for example, to study the participants’ microbiomes, and specifically look for bacteria that earlier studies have found to be associated with insulin resistance. Each participant also filled out a diet questionnaire and took an oral glucose tolerance test, which was used to determine ability to process glucose.
Results..
Investigators found 28 people had oral glucose tolerance results that met the criteria for diabetes. They also found that 135 people had prediabetes, a condition in which a person’s blood-sugar levels are higher than normal but not high enough to meet the definition of diabetes.
The research team analyzed associations between 36 butyrate-producing bacteria found in the stool samples and a person’s ability to maintain normal levels of insulin. They controlled for factors that could also contribute to a person’s diabetes risk, such as age, sex, body mass index and race. Coprococcus and related bacteria formed a network of bacteria with beneficial effects on insulin sensitivity. Despite being a producer of butyrate, Flavonifractor was associated with insulin resistance; prior work by others have found higher levels of Flavonifractor in the stool of people with diabetes.
Investigators are continuing to study samples from patients who participated in this study to learn how insulin production and the composition of the microbiome change over time. They also plan to study how diet may affect the bacterial balance of the microbiome.
SOURCE:
Jinrui Cui, Gautam Ramesh, Martin Wu, Elizabeth T. Jensen, Osa Crago, Alain G. Bertoni, Chunxu Gao, Kristi L. Hoffman, Patricia A. Sheridan, Kari E. Wong, Alexis C. Wood, Yii-Der I. Chen, Jerome I. Rotter, Joseph F. Petrosino, Stephen S. Rich, Mark O. Goodarzi. Butyrate-Producing Bacteria and Insulin Homeostasis: The Microbiome and Insulin Longitudinal Evaluation Study (MILES). Diabetes, August 12 , 2022. Retrieved from : https://diabetesjournals.org/diabetes/article/71/11/2438/147445/Butyrate-Producing-Bacteria-and-Insulin
IMAGE:
https://health.clevelandclinic.org/wp-content/uploads/sites/3/2015/12/GutBacteria-scaled.jpg