Nutrition and Supplements
Probiotics for Parkinson’s Disease
Parkinson’s disease (PD) stands in second place after Alzheimer’s disease among common neurodegenerative disorders. An overall incidence rate of 17 per 100,000 persons per year has been reported. The onset of PD is usually at 65 years or older, and it appears slightly more frequently in men than in women.
The aging of society around the globe is predicted to increase the population affected by PD and result in challenges for the provision of medical and socio-economic care. PD typically is known to be associated with the progressive loss of dopaminergic neurons in substantia nigra pars compacta. Neurons in this region and other brain regions also develop abnormal intracellular deposits known as Lewy bodies that contain aggregated α-synuclein.
Motor impairment, characterized by resting tremor, muscle rigidity and postural instability has long been recognized as hallmarks of PD;however, clinical features of PD include non-motor symptoms, including olfactory dysfunction, pain and sensory disturbances and gastrointestinal (GI) dysfunction.
There have been recent advances in the understanding of PD, where a number of new therapeutic approaches have been introduced. These include genetic and disease-modifying approaches to reduce abnormal accumulation and aggregation of α-synuclein, mitochondrial dysfunction, dysfunction of lysosomal proteins, blockade of neuroinflammation, and enhancement of neurorestoration.
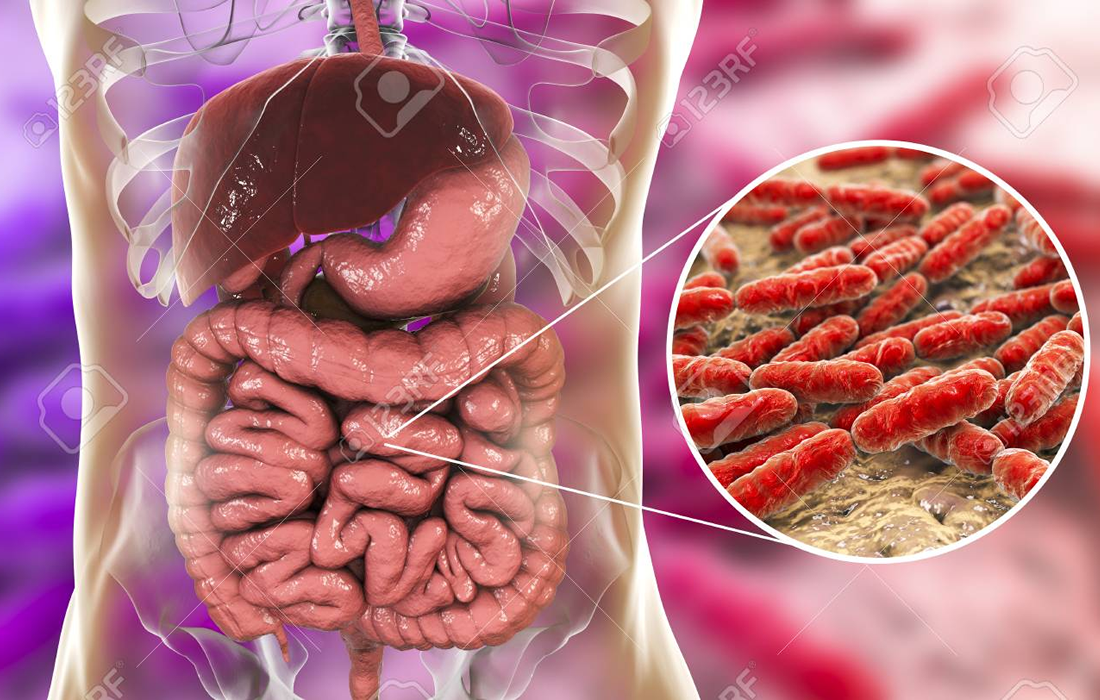
Recently, GI tract, enteric nervous system (ENS), gut microbiota and a cross talk of gut-brain have become a spotlight as a potential mechanism underlying development of PD. An example of how the gut microbiota communicates with the brain is exemplified in the image below:
Human GI tract hosts a diverse population of bacterial species collectively called human gut microbiota, where a symbiosis exists between the host and bacteria. Gut microbiota is influenced by several factors including sex hormones and diet. The latter is influenced by factors such as geographical location and ethnicity, accessibility, and habits.
Maintenance of a healthy microbiota is important for gut barrier integrity, immunity, function, metabolism and the gut-brain axis. Alterations found in gut microbiota, including number and composition of gut microbiota and microbial metabolites, have been considered as valuable signatures for early diagnosis of several neurodegenerative disorders including PD.
GI dysfunction is reported as a potential contributor to PD pathogenesis. This notion is supported by pathophysiologic evidence that α-synuclein inclusions appear early in the ENS then reach the brain.
Emerging evidence suggests that lifestyle factors can contribute to PD pathology. Smoking and coffee have been found associated with reduced risk of PD via their effects on gut microbiota. Probiotics might be a powerful tool in order to alter PD-associated microbiota composition, improve GI function and therefore reduce gut leakiness, bacterial translocation and the associated neuro-inflammation in the ENS.
Some studies have shown that administration of probiotics for 12 weeks resulted in favorable impacts on movement disorders, society-unified Parkinson’s disease rating scale, C reactive protein, blood glutathione and insulin metabolism.
Accumulation evidence supports the contribution of the gut-brain pathway and role of gut microbiota in the development of Parkinson’s disease and other neurodegenerative disorders, which continues under study and could become a potential therapy with a low cost for these types of conditions.
Source:
Gazerani P. Probiotics for Parkinson’s Disease. Int J Mol Sci. 2019;20(17):4121. Published 2019 Aug 23. doi:10.3390/ijms20174121.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6747430/