Stem Cell Therapy for Specific Conditions
Stem Cell Infusion Improves Sepsis Survival in Animal Model
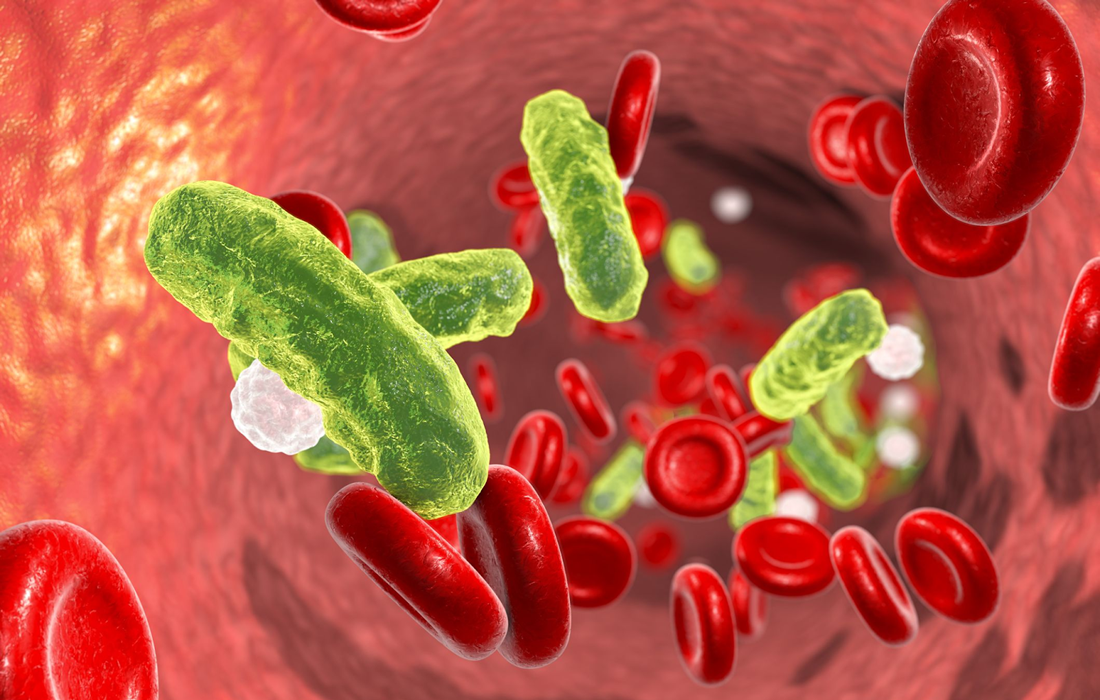
Sepsis accounts for one in five deaths worldwide and is a common final pathway for many disease processes such as cancer, diabetes, and cardiovascular disease. Sepsis is an inflammatory syndrome largely driven by the activation of immune cells by pathogen associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs). After recognizing these molecules via pattern recognition receptors, immune cells become activated and produce proinflammatory cytokines, notably interleukins IL-1, IL-6, interferons (IFNs), and tumor necrosis factor (TNF) that contribute to fever, vasodilation, and multiorgan dysfunction. For patients that progress to septic shock, mortality rates remain as high as 40%.
Leukopenia is a feature of severe sepsis that arises from apoptosis of peripheral immune cells and is an independent risk factor for death. To counteract the adverse effects of leukopenia, investigators have used immunotherapies such as GM-CSF or granulocyte infusions in an attempt to restore leukocyte numbers and improve survival.
Recents studies indicate that hematopoietic stem and progenitor cells (HSPCs) express surface receptors for cytokines, chemokines, and PAMPs , and respond rapidly upon direct and indirect stimulation by these signals. The capacity of HSPCs to directly detect pathogen-derived molecules, cytokines, and chemokines suggests that emergency granulopoiesis can be mobilized from even the most primitive hematopoietic progenitors and that HSPCs have an active role in fighting infections. However, the extent and mechanism by which HSPC responses contribute to immunity in the acute setting remain poorly defined.
A one-time infusion of stem cells from bone marrow improves the survival of mice with sepsis
First, the team examined the effects of sepsis on mice following infection with Streptococcus pyogenes, the pathogen that causes strep throat. They found that a detrimental effect of the condition is a severe drop in the number of hematopoietic stem and progenitor cells (HSPCs) in the animals’ bone marrow. These cells are responsible for the day-to-day production of all blood and immune cells.
The team suspected that the number of HSPCs drops because the cells work overtime to produce the immune and blood cells needed to fight both the infection and the severe inflammation caused by sepsis.
Following this discovery, the researchers investigated whether an infusion of new healthy HSPCs could improve sepsis outcomes. To answer this question, they gave mice with sepsis an infusion of approximately 10,000 healthy new HSPCs around 24 hours following infection. The treatment increased the animals’ survival by 50-60% compared with mice that did not receive an HSPC infusion. This treatment also decreased the number of inflammatory molecules called cytokines in the animals.
Surprisingly, we found that HSPC infusion did not reduce the amount of bacteria in the mice.
Currently, clinicians sometimes transfuse a different type of immune cell, called granulocytes, to treat sepsis patients with depleted immune cells. But these transfusions offer a limited benefit to patients. Additionally, granulocyte transfusions require large numbers of donor cells and must be given repeatedly.
SOURCE:
Daniel E Morales-Mantilla, Bailee Kain, Duy Le, Anthony R Flores, Silke Paust, Katherine Y King. Hematopoietic stem and progenitor cells improve survival from sepsis by boosting immunomodulatory cells. eLife, 2022; 11 DOI: 10.7554/eLife.74561
IMAGE:
https://hips.hearstapps.com/hmg-prod/images/sepsis-1527871947.jpg