Stem Cell Therapy for Specific Conditions
Stem Cell Therapy for Hypoxic-ischemic Encephalopathy
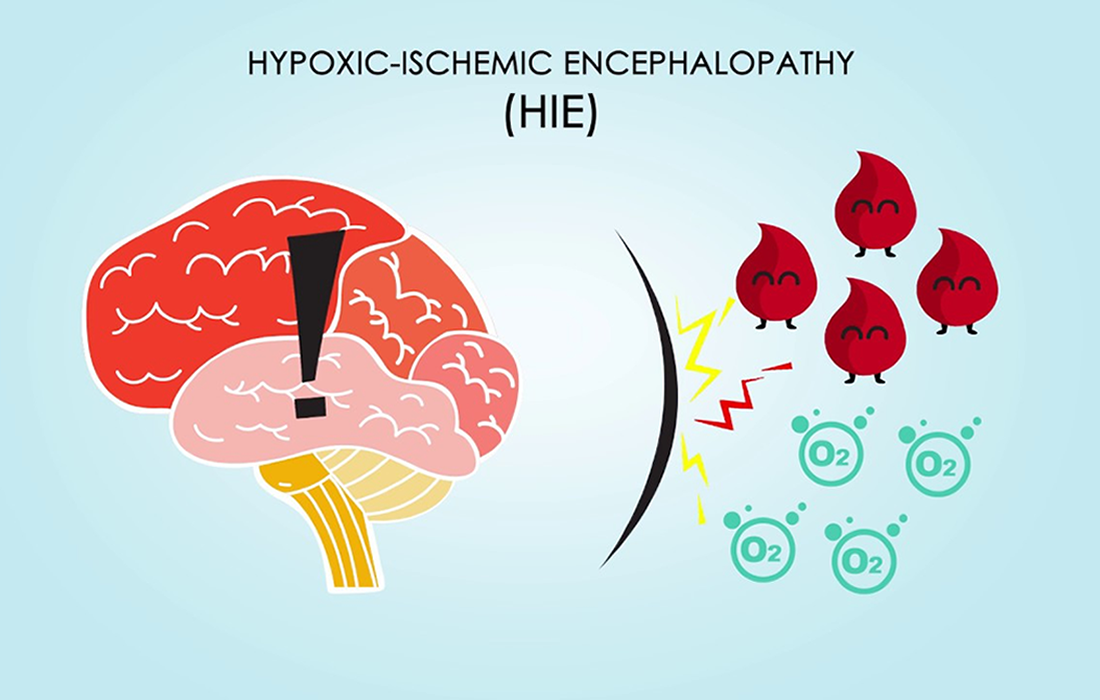
What is Hypoxic-ischemic Encephalopathy?
Hypoxic ischemic encephalopathy (HIE) is a serious birth complication affecting full term infants: 40%–60% of affected infants die by 2 years of age or have severe disabilities. It occurs in 1.5 -2.5 per 1000 live births in developed countries. The majority of the underlying pathologic events of HIE are a result of impaired cerebral blood flow and oxygen delivery to the brain with resulting primary and secondary energy failure. In the past, treatment options were limited to supportive medical therapy.
Epidemiology
The incidence of HIE has not declined even with advances in obstetric care (i.e. fetal monitoring) aimed at preventing the hypoxic-ischemic event; thus much of the current neonatal research about HIE focuses on minimizing the extent of subsequent brain injury. In the past, treatment options were limited to supportive medical therapy to maintain cardiopulmonary function and to manage seizure activity. Currently, several experimental treatments are available to infants with HIE and many others are being evaluated in animal models.
What Causes HIE?
HIE is a disorder in which clinical manifestations indicate brain dysfunction. While the exact cause is not always identified, antecedents include cord prolapse, uterine rupture, abruptio placenta, placenta previa, maternal hypotension, breech presentation, or shoulder dystonia.
The manifestations of perinatal HIE in early postnatal life include:
- Abnormal fetal heart rate tracings.
- Poor umbilical cord gases.
- Low Apgar scores.
- Presence of meconium stained fluid.
- Need for respiratory support within the first several minutes of postnatal life.
The majority of the underlying pathologic events of HIE are a result of impaired cerebral flow and oxygen delivery to the brain.
Treatment Options
The uses of neuroprotective agents for primary energy failure being explored are limited to preconditioning the cerebral tissue to require low levels of oxygen prior to the hypoxic-ischemic event. Some of the therapies being used are:
- Moderate hypothermia. This is the most prominent emerging treatment for infants with HIE. Hypothermia is thought to be effective because it reduces free radicals and glutamate levels, decreases oxygen demand and decreases apoptosis.
Hypothermia treatment is delivered through either selective head or whole body cooling of the infant. Hypothermia treatment involves decreasing the infant’s body temperature to between 33°C and 36.5°C. Infants are generally cooled for 48 to 72 hours and then rewarmed slowly to prevent complications. - Erythropoietin. Erythropoietin (EPO) is a glycoprotein hormone responsible for erythropoiesis. Endogenous EPO is generally thought to be produced by the kidneys to stimulate erythropoiesis; however, EPO is also produced by astrocytes, neurons, and oligodendrocytes near the site of injury.
The exact mechanisms of neuroprotective mechanisms of exogenous EPO remain unknown, but appear to be related to inhibition of neuronal apoptosis in the hippocampus, reduction of glial activation (immune system) and reduction in primary brain edema.
Recently, in addition to supportive therapy and symptomatic treatment, research on the treatment of HIE has focused on the following aspects: hypothermia therapy, neuroprotective agents, etc. Another new therapeutic tool with promising indications for clinical practice is stem cell therapy.
Mesenchymal Stem Cell Therapy
There is ever increasing evidence on mesenchymal stem cells (MSCs), suggesting that they promote the improvement of neurological functions with significant immunomodulatory effects against neuroinflammatory events. Bone marrow-derived MSCs (BM-MSCs) and umbilical cord blood-derived MSCs are now being included in efforts to prevent ischemic brain damage. Fetal-derived MSCs, which are more primitive and have less immune reactivity, have recently been suggested as better alternatives for BM-MSCs. Thus, Wharton’s jelly-derived MSCs (WJ-MSCs) can easily be obtained in abundance and are readily cultured, making them good alternatives.
Kabataş, et al, investigated the safety and preliminary efficacy of allogenic mesenchymal stem cells (MSCs) in HIE patients. They studied 8 patients with a mean age of 33± 10 years and did triple route (Intravenous, intrathecal and intramuscular administration) Wharton’s jelly derived MSC administrations. They evaluated the patients prior and after treatments with two scales: Modified Ashworth (MA) scale, which measures clinically the spasticity in patients with neurological conditions, and with the Functional Independence Measure (FIM) which provides an uniform system to measure disability and how much assistance the patient requires in daily living activities.
Patients showed good tolerance with no severe side effects associated with the administration of the cells. There were no problems of safety or side effects during the 1 year follow up.
The most significant finding in their study was the 12 point increase in the FIM Motor scores, which could prove substantial if confirmed by further research. At baseline, 14.28% of patients had a FIM Motor score of 91, which increased to 14.7 in the first month and 19.37 in the first year.
The patients also had significant improvement in FIM Cognitive scores over the course of a year, indicating long term impact on brain functions.
One added benefit of using Warthon’s jelly derived mesenchymal stem cells is that they do not require immunosuppression because they are more primitive and have less immune reactivity, as compared to other types of cells like those derived from bone marrow.
More studies with larger populations are needed to verify the safety and efficacy outcomes obtained in this study; however the positive results show us the promising and potential benefit of regenerative therapies.
Source:
Kabataş S, Civelek E, Kaplan N, Savrunlu EC, Sezen GB, Chasan M, Can H, Genç A, Akyuva Y, Boyalı O, Diren F, Karaoz E. Phase I study on the safety and preliminary efficacy of allogeneic mesenchymal stem cells in hypoxic-ischemic encephalopathy. World J Exp Med 2021; 11(2): 17-29.
Allen KA, Brandon DH. Hypoxic Ischemic Encephalopathy: Pathophysiology and Experimental Treatments. Newborn Infant Nurs Rev. 2011;11(3):125-133.
Image from: