Stem Cell Therapy for Specific Conditions
Stem Cell Therapy for Lupus
What is Lupus?
Systemic lupus erythematosus (SLE) is a systemic autoimmune disease that is characterized by autoantibodies with immune complex deposition leading to multiorgan injury. Is a disease that occurs when your body’s immune system attacks your own tissues and organs (autoimmune disease). Inflammation caused by lupus can affect many different body systems, including your joints, skin, kidneys, blood cells, brain, heart and lungs.
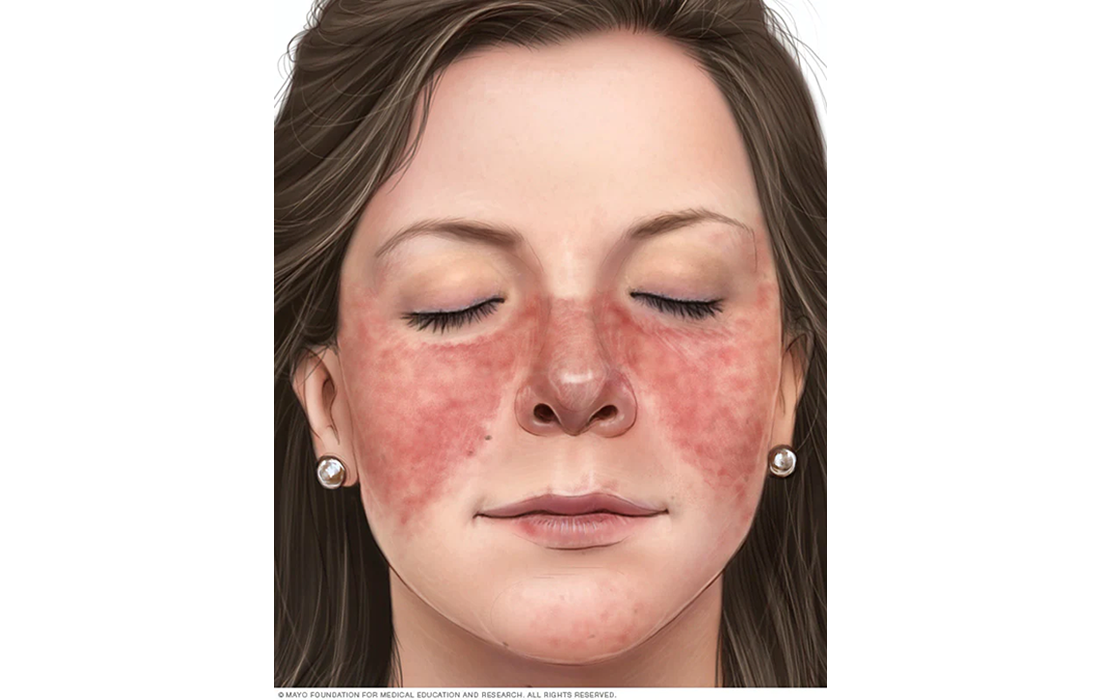
Lupus can be difficult to diagnose because its signs and symptoms often mimic those of other conditions. The most distinctive sign of lupus is a facial rash that resembles the wings of a butterfly unfolding across both cheeks; it can occur in many but not all cases.
In spite of the significant variation of disease severity among SLE patients, the dysregulation of innate and adaptive immune responses are universal.
What Causes Lupus?
As an autoimmune disease, it occurs when your immune system attacks healthy tissue in your body. It is likely that the disease results from a combination of genetics and environmental factors.
Some people are born with a tendency toward developing lupus, which may be triggered by infections, certain drugs or even sunlight. While there’s no cure for lupus, treatments can help control symptoms. Some potential triggers include:
- Sunlight. Exposure to the sum may bring on lupus skin lesions or trigger an internal response in susceptible people.
- Medications. Lupus can be triggered by certain types of blood pressure medications, anti-seizure drugs and antibiotics. Drug induced lupus usually get better when the patient stops taking the medication. Rarely, symptoms may persist even after the drug is stopped.
- Infections. Having an infection can initiate lupus or cause a relapse in some people.
What are Common Signs and Symptoms?
Every lupus case is different. Signs and symptoms may come on suddenly or develop slowly, may be mild or severe, and may be temporary or permanent. Most people with lupus have mild disease characterized by episodes, called flares, when signs and symptoms get worse for a while, then improve or even disappear completely for a time.
The signs and symptoms depend on which area or system is being affected by lupus, which can vary in every case. Some of the most commons are:
- Fatigue.
- Weight loss.
- Joint pain, stiffness and swelling.
- Butterfly-shaped rash on the face.
- Skin lesions that appear or worsen with sun exposure.
- Fingers and toes that turn white or blue when exposed to cold or during stress, called Raynaud’s phenomenon.
- Shortness of breath or chest pain.
- Dry eyes.
Patients at high risk for lethal complications may be identified by renal disease, hypertension, lung involvement, anemia, thrombocytopenia, and antibodies to phospholipids, or active disease demonstrated by a high disease activity index score despite therapy.
Current Treatment Options
Treatment for lupus depends on your signs and symptoms. The medications most commonly used to control lupus include:
- Nonsteroidal antiinflammatory drugs (NSAIDs). Over-the-counter NSAIDs such as naproxen and ibuprofen may be used to treat pain, swelling and fever associated with lupus. They can cause many side effects including stomach bleeding, kidney damage and increased risk of heart problems.
- Antimalarial drugs. Medications used to treat malaria such as hydroxychloroquine (Plaquenil), affect the immune system and can help decrease the risk of flares.
- Corticosteroids. Prednisone and other types can counter the inflammation of lupus. High doses of steroids like methylprednisolone (Medrol) are often used to control serious diseases that involve the kidneys and brain. They can cause major side effects, including osteoporosis, high blood pressure, diabetes, increased risk of infection and weight gain.
- Immunosuppressants. Drugs that suppress the immune system are also commonly used. Some examples include azathioprine (Imuran), methotrexate, cyclosporine and leflunomide. Potential side effects include increased risk of infection, liver damage, decreased fertility and increased risk of cancer.
- Biologics. Belimumab (Benlysta) administered intravenously reduces lupus symptoms in some people. This type of medications are derived or synthesized from living biological organisms.
Use of Cellular Therapies
Stem cell therapy is one of the most promising frontiers in lupus research today, especially for people whose lupus doesn’t respond to other treatments (called refractory lupus).
Mesenchymal stem cells (MSCs) possess immunomodulatory properties and functions to immune cells, including T, B NK cells and macrophages. MSCs regulate the dendritic cells (DC) function by inhibiting their co-stimulatory molecule expression and proinflammatory cytokine production, leading to the suppression of their capacity to initiate naive T cells and immune responses.
A study published in the journal Nature Communications in 2019 by Xinran Yuan and colleagues used allogeneic Umbilical cord MSCs (UC-MSCs) to evaluate their use for lupus treatment.The patients were refractory to treatment and lacked response to conventional immunosuppressive drugs.
In the study 21 patients underwent UC-MSCs transplantation. All patients underwent U-MSCT and one million cells per kilogram of body weight were administered by intravenous infusion, without adding steroid or other immunosuppressive drugs. After the transplantation, the doses of steroids as well as immunosuppressive drugs were tapered according to the amelioration of disease conditions. No adverse reactions were reported. They saw decreased disease activity, with remission in 2 patients and about half of them had a partial remission.
Another clinical study conducted by Jun Liang. et al. found that allogeneic stem cell therapy significantly reduced disease activity in Lupus patients.
The study included 15 patients with persistently active Systemic lupus erythematosus (SLE). The outcome was evaluated by changes in the SLE disease activity index (SLEDAI), serological features (anti-nuclear antibodies and anti-double-stranded DNA (anti-dsDNA)), renal function and percentage of peripheral blood regulatory T cells.
Stem Cell Therapy at Zignagenix
Mesenchymal stem cells have the ability to modulate the immune system. Due to the nature of this condition and how it’s caused by a dysregulation in the immune system, MSCs are an excellent treatment option that has been under study and has shown good results.
At our clinic we use MSCs derived from the Warthon’s jelly umbilical cord at high doses infused intravenously (IV) combined with exosomes to increase the effectiveness of the therapy.
We also combine the IV therapy with localized injections on cases of Lupus with affectation to joints to decrease the local inflammation in the intra-articular space. By injecting stem cells directly into the joint space the MSCs can modulate the immune response locally to decrease the inflammation and can also help regenerate some of the damaged tissue. By doing so patients can decrease the degree of pain and joint edema that can sometimes occurs lupus.
Sources:
https://www.mayoclinic.org/diseases-conditions/lupus/symptoms-causes/syc-20365789
Yuan, X., Qin, X., Wang, D. et al. Mesenchymal stem cell therapy induces FLT3L and CD1c+ dendritic cells in systemic lupus erythematosus patients. Nat Commun 10, 2498 (2019). https://doi.org/10.1038/s41467-019-10491-8
Burt, R., Marmont, A., Arnold, R. et al. Development of a phase III trial of hematopoietic stem cell transplantation for systemic lupus erythematosus. Bone Marrow Transplant 32, S49–S51 (2003). https://doi.org/10.1038/sj.bmt.1703943
Jayne D, et al. Autologous stem cell transplantation for systemic lupus erythematosus. Lupus. 2004;13(3):168-76. doi: 10.1191/0961203304lu525oa.
Liang J, Zhang H, Hua B, et alAllogenic mesenchymal stem cells transplantation in refractory systemic lupus erythematosus: a pilot clinical studyAnnals of the Rheumatic Diseases 2010;69:1423-1429.
Image from:
Mayo Foundation for Medical Education and Research
https://www.mayoclinic.org/diseases-conditions/lupus/symptoms-causes/syc-20365789