Stem Cell Therapy for Specific Conditions
Stem Cell Therapy for Osteoporosis
What is Osteoporosis?
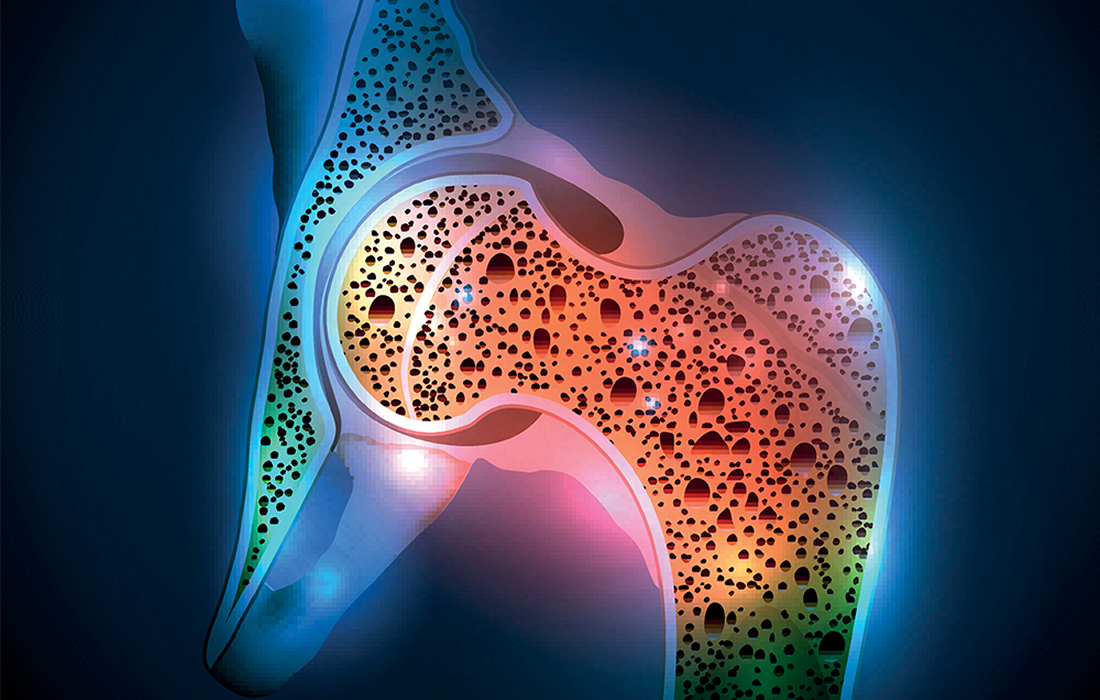
Osteoporosis is a systemic skeletal disease that is characterized by low bone mass and microarchitectural deterioration of the bone tissue. It affects 44 million Americans and more than 200 million people worldwide.
The main characteristics of osteoporosis are bone loss and microstructural degeneration. It causes the bones to become weak and brittle, so brittle that a fall or even mild stresses such as bending over or coughing can cause a fracture. The most common areas of fractures occur in the hip, wrist, or spine.
Bone is living tissue that is constantly being broken down and replaced. Osteoporosis occurs when the creation of new bone doesn’t keep up with the loss of old bone.
Osteoporosis affects men and women of all races. But white and Asian women, especially older women who are past menopause, are at the highest risk. Medications, a healthy diet, and weight-bearing exercise can help prevent bone loss or strengthen already weak bones.
What are common Signs and Symptoms?
There typically are no symptoms in the early stages of bone loss. But once the bones have been weakened by osteoporosis, you might have signs and symptoms that include:
- Back pain, caused by a fractured or collapsed vertebra.
- Loss of height over time.
- A stooped posture.
- A bone that breaks much more easily than expected.
What Causes Osteoporosis?
The pathogenesis of osteoporosis stems from an improper balance between the processes of bone formation, carried out by the osteoid-secreting osteoblast, and bone resorption, achieved by the proteolytic bone-digestive osteoclast.
Different factors can contribute to disease development, such as behavioral, nutritional, hormonal, and genetic predisposition. However, the incidence is most common in postmenopausal women, in which the rate of bone turnover dramatically increases with estrogen deficiency and results in continuous bone loss.
Medical conditions that can increase the risk of osteoporosis are:
- Celiac disease.
- Inflammatory bowel disease.
- Cancer.
- Kidney or liver disease.
- Multiple myeloma.
- Rheumatoid arthritis.
Some dietary factors that can contribute to the development of the disease are:
- Low calcium intake. A lifelong lack of calcium plays a role in the development of osteoporosis. Low calcium intake contributes to diminished bone density, early bone loss, and increased risk of fractures.
- Eating disorders. Severely restricting food intake weakens bone in both men and women.
- Gastrointestinal surgery. Surgery to reduce the size of the stomach or removal of part of the intestine can limit the amount of surface to absorb nutrients, including calcium.
Current Treatment Options
Treatment recommendations are often based on an estimate of the risk of having a fracture in the next 10 years using information such as the bone density test. If the risk is low the treatment often focuses on preventive measures such as lifestyle modifications. When it is high, treatment includes medication.
One of the most commonly used therapeutic agents is bisphosphonates, which inhibit bone resorption by triggering apoptosis in osteoclasts. Although bisphosphonate therapy reduces the risk of osteoporotic-related fractures, it has been associated with serious side effects, such as osteonecrosis of the jaw and atypical femoral fractures.
Other agents that reduce bone loss and minimize fracture risk include the selective estrogen receptor modulators (SERMs), calcitonin, and receptor activator of nuclear factor kappa B ligand (RANKL) inhibitors, such as the human monoclonal antibody denosumab.
Another treatment option is hormone-related therapy. The use of estrogen, especially when started soon after menopause, can help maintain bone density. However, estrogen therapy can increase the risk of breast cancer and blood clots, which can cause strokes. Therefore, estrogen is typically used for bone health in younger women or in women whose menopausal symptoms also require treatment.
Regenerative Medicine Therapy
Stem cell therapy has been studied for its many capabilities in tissue regeneration. Stem cells are introduced into tissues to repair, replace, and treat a defect. They are undifferentiated biological entities with the capacity to self-renew and differentiate into specialized cell types.
Mesenchymal stem cells (MSCs) are multipotent stromal cells and are the most commonly used stem cells in the current preclinical and clinical studies on skeletal diseases.
MSCs are of great importance because of their paracrine effects through secreting growth factors and cytokines, such as vascular endothelial growth factor (VEGF), transforming growth factor-beta (TGF-β), and interleukins (IL-1β, IL-6, and IL-8).
In a clinical trial by Lozano-Rivas and colleagues on new osteoporotic fractures, reduced pain was seen in patients with osteoporosis following autologous intravenous (IV) infusion of bone marrow MSCs.
Another trial by Hendrijantini and colleagues evaluated the use of human umbilical cord-derived mesenchymal stem cells (hUC-MSCs) in a rat model with ovariectomy-induced osteoporosis. The rats received hUC-MSCs and showed a higher bone mass, collagen content, and osteoblasts number, while the number of osteoclasts decreased in the implantation site. Also, an in vitro study confirmed that hUC-MSCs promote osteoblasts formation while preventing the cellular activity of osteoclasts.
In a study from the Ottawa Hospital Research Institute in Ontario, Canada, researchers show that MSCs can be extremely useful in the treatment of osteoporosis. They used the Sca-1 null mouse model of human type II osteoporosis (a type of osteoporosis that occurs in men and women who are more than 75 years old, with cortical and trabecular bone loss) and showed that minimally expanded unmodified donor MSCs can prevent the progression of osteoporosis-associated symptoms, and so may have relevance in the treatment of the human form of the disease.
Conclusions
As we can see the use of regenerative medicine for the treatment of osteoporosis continues to be investigated due to the promising results that different animal studies have shown with an increase in bone mass, collagen content, a decrease in pain, increased number of osteoblasts, which are the bone-forming cells and decrease in the number of osteoclasts, which are in charge of bone resorption and contribute to the development of the disease.
More and larger clinical studies are needed in order to know if the results can translate to the human model of osteoporosis, but the current evidence shows that it could become an excellent therapeutic option in the near future.
Sources:
https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968
Antebi, B., Pelled, G. & Gazit, D. Stem Cell Therapy for Osteoporosis. Curr Osteoporos Rep 12, 41–47 (2014). https://doi.org/10.1007/s11914-013-0184-x
Jiang, Y., Zhang, P., Zhang, X., Lv, L., & Zhou, Y. (2021). Advances in mesenchymal stem cell transplantation for the treatment of osteoporosis. Cell proliferation, 54(1), e12956. https://doi.org/10.1111/cpr.12956
Kangari, P., Talaei-Khozani, T., Razeghian-Jahromi, I. et al. Mesenchymal stem cells: amazing remedies for bone and cartilage defects. Stem Cell Res Ther 11, 492 (2020). https://doi.org/10.1186/s13287-020-02001-1
Stuart P. Atkinson (2016, May 29). Can a Single Dose of MSCs be an Effective Treatment for Osteoporosis? Stem Cells Portal. Retrieved from:
https://stemcellsportal.com/article-scans/can-single-dose-mscs-be-effective-treatment-osteoporosis
Image from: