Stem Cell Therapy for Specific Conditions
Stem Cell Therapy for Tye 1 Diabetes Mellitus
What is Type 1 Diabetes Mellitus?
Type 1 diabetes mellitus (T1DM) is the most common chronic autoimmune disease in young patients and is characterized by the loss of pancreatic β cells; as a result, the body becomes insulin deficient and hyperglycemic.
In type 1 diabetes mellitus, autoimmune destruction of pancreatic islet b cells reduces an individual’s ability to regulate blood glucose, ultimately resulting in poor blood circulation, heart disease, stroke, infection, kidney failure and often premature death.
Although hyperglycemia can be ameliorated by drugs or exogenous insulin administration, these treatments cannot provide physiological regulation of blood glucose. Therefore, the ideal treatment for diabetes should restore both insulin production and insulin secretion regulation by glucose in patients.
Every day millions of patients with T1DM receive insulin injections to survive, but these injections do nothing to address the underlying T cell-mediated autoimmune dysfunction. For over 2 decades, attempts to address the underlying autoimmunity have been unsuccessful due to the polyclonal nature of the autoimmune response.
Different factors, including genetics and some viruses, may contribute to type 1 diabetes. Although type 1 diabetes usually appears during childhood or adolescence, it can develop in adults.
Despite active research, type 1 diabetes has no cure. Treatment focuses on managing blood sugar levels with insulin, diet and lifestyle to prevent complications.
Symptoms of Type 1 Diabetes Mellitus
- Increased thirst.
- Frequent urination.
- Bed-wetting in children who previously didn’t wet the bed during the night.
- Extreme hunger.
- Unintended weight loss.
- Irritability and other mood changes.
- Fatigue and weakness.
- Blurred vision.
Stem Cell Therapy and Clinical Trials
Stem cells have been touted as a means of replacing lost pancreatic islet β cells and curing T1DM. Human cord blood derived stem cells (CB-SCs) and mesenchymal stem cells have been shown to modulate immune activity in vitro and subsequent studies have demonstrated that CB-SCs can be used to alter immune function and improve markers of T1DM in mouse models. They are also able to modulate the immune function of T1DM patient-derived islet β cell-specific pathogenic T cell clones.
In the last few years, controlled clinical trials have been carried out to estimate the efficiency and safety of stem cell therapy for T1DM. It has been demonstrated that MSCs can ameliorate or reverse the manifestation of diabetes in animal models of T1DM.
Stem cell-based strategies represent significant therapeutic potential owing to the immunomodulatory potential and differentiation potentials of stem cells. These properties can potentially prevent β cell destruction, preserve residual β cell mass, and facilitate β cell regeneration.
A study performed at the Stem Cell Research Center in Qingdao University, China studied the long term effects of the implantation of Wharton’s jelly derived mesenchymal stem cells (WJ-MSCs) from the umbilical cord in newly-onset T1DM patients. 29 patients were divided in 2 groups, one treated with WJ-MSCs and another one with insulin intensive therapy. No adverse effects were reported. They found that in the group treated with stem cells the HbA1c levels decreased compared to the control group and C-peptide increased in the group treated with stem cells also, which suggested that the treatment is safe and effective.
During January 2009 and December 2010, in a clinical trial, 42 patients aged 18-40 years with a history of T1DM for ≥ 2 years and ≤ 16 years were randomized into either the stem cell transplantation were randomized into either stem cell transplantation with umbilical cord stem cells or standard insulin treatment groups.
After 1 year a follow up was performed indicating that the C-peptide increased in treated patients, whereas it decreased in control groups; insulin also increased in treated patients; and it decreased from in control patients.
Additionally, HbA1c and fasting glycemia decreased in the treated groups and increased in the control subjects. Daily insulin requirements in the treated groups also decreased compared to those of the control groups.
What is C-peptide?
C-peptide is the part of proinsulin which is cleaved prior to co-secretion with insulin from pancreatic beta cells. C-peptide and insulin are released from the pancreas at the same time and in about equal amounts. So a C-peptide test can show how much insulin your body is making.
A C-peptide test is often used to help tell the difference between type 1 and type 2 diabetes. With type 1 diabetes, your pancreas makes little to no insulin, and little or no C-peptide. With type 2 diabetes, the body makes insulin, but doesn’t use it well. This can cause C-peptide levels to be higher than normal.
Conclusions
Stem cell therapy has been considered a promising potential therapeutic method for diabetes treatment, especially for T1DM due to its immunological component and the immunomodulatory and regenerative capabilities of stem cells. The application of stem cell-based therapy for T1DM represents the most advanced approach for curing type 1 diabetes.
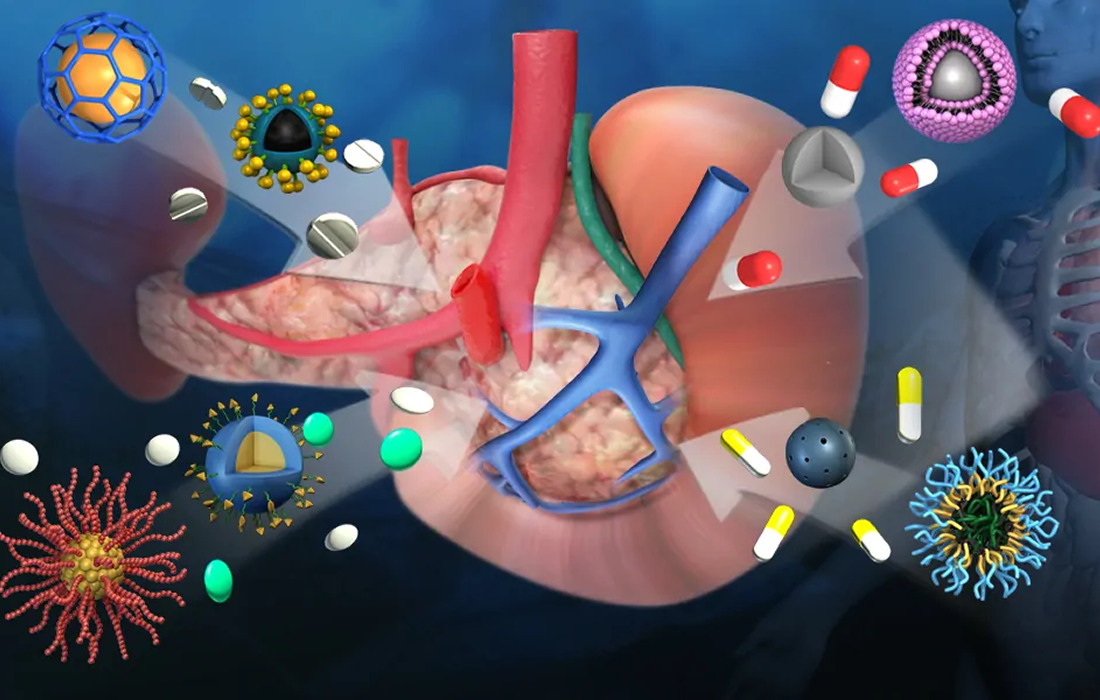
At Zignagenix we use WJ-MSCs to treat these conditions with excellent results. Patients can see an increase in their quality of life, decrease dosage utilization of insulin and a better metabolic glycemic control. The therapy is performed with high doses of mesenchymal stem cells infused intravenously and is combined with exosomes to increase the efficacy of the therapy.
Sources:
Zhao Y, Jiang Z, Zhao T, et al. Reversal of type 1 diabetes via islet β cell regeneration following immune modulation by cord blood-derived multipotent stem cells. BMC Med. 2012;10:3. Published 2012 Jan 10.
Chen S, Du K, Zou C. Current progress in stem cell therapy for type 1 diabetes mellitus. Stem Cell Res Ther. 2020;11(1):275. Published 2020 Jul 8. doi:10.1186/s13287-020-01793-6
Shi-Yi Sun, et al. Efficacy and Safety of Stem Cell Therapy for T1DM: An Updated Systematic Review and Meta-Analysis. Journal of Diabetes Research. Volume 2020, Article ID 5740923, 12 pages. https://doi.org/10.1155/2020/5740923
J. Hu, X. Yu, Z. Wang et al., “Long term effects of the implantation of Wharton’s jelly-derived mesenchymal stem cells from the umbilical cord for newly-onset type 1 diabetes mellitus,” Endocrine Journal, vol. 60, no. 3, pp. 347–357, 2013.
https://www.mayoclinic.org/diseases-conditions/type-1-diabetes/symptoms-causes/syc-20353011
Image from: https://www.advancedsciencenews.com/earlier-diagnosis-for-type-1-diabetes/