Stem Cell Therapy for Specific Conditions
Stem Cell Therapy Shows Promise for Pulmonary Arterial Hypertension
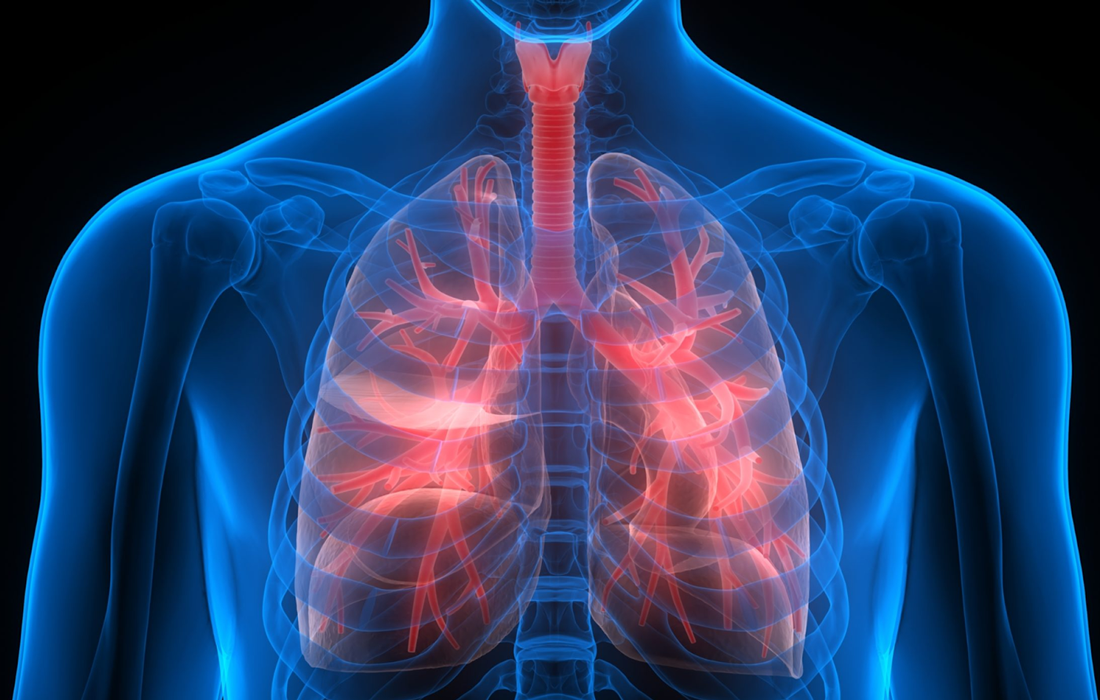
Pulmonary arterial hypertension (PAH) is a devastating disease that is caused by a progressive increase in pulmonary vascular resistance, largely because of severe remodeling of distal lung arterioles. By definition, pulmonary hypertension refers to the condition in which resting mean pulmonary arterial pressure (mPAP) is greater than 25 mmHg.
Etiology
The strict definition of PAH is pulmonary hypertension with no known cause. However, associations have been recognized (eg, connective-tissue diseases, liver cirrhosis, exposure to anorexigens and likely other alpha-adrenergic stimulants [eg, cocaine, amphetamines], HIV infection). How these associated conditions predispose to or cause PAH remains unknown.
Epidemiology
PAH is responsible for approximately 125-150 deaths per year in the United States and has an incidence rate of approximately 2-6 cases per million population per year. In the United States, the average female-to-male ratio reported in clinical trials and registries is close to 4:1. The reasons for this female predilection remain unknown.Typically, younger women of childbearing age develop PAH. However, PAH can also affect individuals in their fifth and sixth decades of life or older.
Treatment
Treating IPAH requires significant education regarding, and exposure to, the available therapies for IPAH and their potential complications. Because IPAH is relatively rare, management is best left to expert personnel at centers with regular exposure to these patients.
Until about 15 years ago, calcium channel blockers (CCBs) had been the most widely used class of drugs for PAH. These drugs are thought to act on the vascular smooth muscle to dilate the pulmonary resistance vessels and lower the pulmonary artery pressure. Several studies report clinical and hemodynamic benefits from the use of long-term calcium channel blockade.
Other approaches include low-sodium and low-fluid diet, and physical activity recommendation to improve the prognosis and quality of life of the patients.
Prognosis
IPAH has no cure. Untreated IPAH leads to right-sided heart failure and death. Prior to the 1990s, therapeutic options were limited. The emergence of novel drug therapies has greatly improved the outlook for patients with PAH and PAH-like diseases.
For untreated IPAH, the estimated 3-year survival rate is approximately 41%. In one study of long-term continuous intravenous prostacyclin therapy, 3-year survival increased to approximately 63%.
Stem cell therapy could be a promise to treat PAH
Canadian researchers have published promising results of the first clinical trial in the world of a genetically-enhanced stem cell therapy for pulmonary arterial hypertension (PAH).
Dr. Duncan Stewart, senior author of the paper, senior scientist at The Ottawa Hospital and professor of medicine at the University of Ottawa, and his team analized the feasibility and side effects of a genetically-enhanced stem cell therapy to repair and regenerate lung blood vessels in PAH.
Seven patients underwent a blood cell selection process (apheresis) to harvest a certain population of their white blood cells. These cells were then grown in the laboratory under special conditions to select for stem-like cells called endothelial progenitor cells. These cells were genetically engineered to produce greater amounts of nitric oxide, a natural substance that widens blood vessels and is essential for efficient vascular repair and regeneration. The genetically enhanced cells were then injected directly into the lung circulation of the same patient.
The researchers did observe that patients had improved blood flow in the lungs in the days following the therapy, and enhanced ability to exercise and better quality of life for up to six months after the therapy.
The therapy was generally well-tolerated, however one patient who had very severe disease and signs of poor prognosis died one day after treatment.
Conclusions
This trial shows that genetically-enhanced stem cell therapy is a promising treatment approach for pulmonary arterial hypertension. Although this is an important start, it is necessary to do larger studies to establish whether this therapy can produce important and durable benefits for people suffering from this challenging disease. Another thing that it is necessary to considerate is the placebo group, to know for sure if the effects observed were due to the cells or to psychological effects.
SOURCE:
John Granton, David Langleben, Michael J Kutryk, Nancy Camack, Jacques Galipeau, David Courtman, Duncan J Stewart, (July 20, 2015). Endothelial NO-Synthase Gene-Enhanced Progenitor Cell Therapy for Pulmonary Arterial Hypertension: the PHACeT Trial. Circulation Research. Retrieved from : https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.114.305951
https://emedicine.medscape.com/article/301450-overview#a7
IMAGE:
https://www.inovanewsroom.org/wp-content/uploads/2017/05/shutterstock_396426208.jpg