Platelet-Rich Plasma
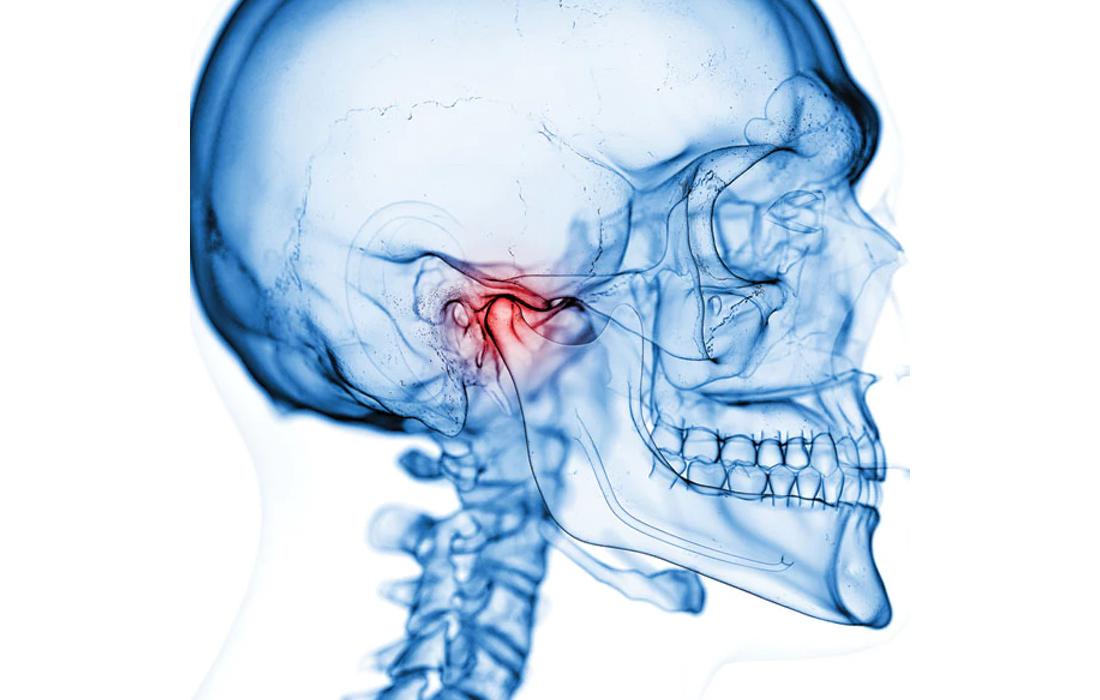
Temporomandibular Joint Disorders and the use of PRP
Temporomandibular joint disorders (TMDs) affect the jaw joints and related structures causing internal derangement of joint space, bone alterations and degenerative pathologies. Frequent signs and symptoms of TMDs are pain, joint noise, limited range of motion, impaired jaw function, deviation or deflection upon mouth opening and closing or open locking.
Some changes may include disc displacements, often responsible for joint sounds, pain and discomfort in the TMJ area. They generally are related to the structure and cinematics of the joint and masticatory system, but can also be caused by anatomical morphology of the condyle, glenoid fossa and articular eminence. Furthermore, age, dentition and patterns of masticatory muscle could be important in determining or maintaining dislocations.
Osteoarthritis of the TMJ is characterized by degenerative changes in the bone, cartilage and supporting tissues causing pain, stiffness and loss of function. It is more common in females than males. In most cases there is a limitation in motion and patients are not able to chew effectively or achieve a normal mouth opening without pain, which decreases their quality of life.
Some treatments available include painkillers, resting the jaw, splints and physiotherapy and surgical interventions as arthrocentesis, disc repositioning or discectomy in patients that don’t respond to conservative therapy.
A treatment that has been under study in recent years is the use of Platelet-rich Plasma due to its anti-inflammatory, analgesic and antibacterial properties. PRP has recently been considered as an ortho-biological adjuvant treatment. It can restore intra-articular hyaluronic acid, increase glycosaminoglycan chondrocyte synthesis, angiogenesis and promote stem cell migration.
Differents studies suggest that PRP injection could improve the metabolic changes that occur in TMDs (changes in microenvironment around cartilage and bone), by expanding the joint cavity, restoration of disc, capsule and retrodiscal pad by growth factors and the inhibition of pro-inflammatory cytokines.
Hegab, et al. showed that PRP injections are comparable and even better than Hyaluronic acid injections at long term follow ups without recurrence of pain or joint sound at 12 months.
Source:
Zotti F, Albanese M, Rodella LF, Nocini PF. Platelet-Rich Plasma in Treatment of Temporomandibular Joint Dysfunctions: Narrative Review. Int J Mol Sci. 2019;20(2):277. Published 2019 Jan 11. doi:10.3390/ijms20020277
Source link: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6358929/