Regenerative Medicine News and General Information
Airway Inflammation and COPD are More Common in Marijuana Smokers than Cigarette Smokers, a Study Suggest
Marijuana is the most widely used illicit psychoactive substance in the world and the second-most commonly smoked substance after tobacco. Its use has increased in Canada since the legalization of nonmedical marijuana in 2018. In 2020, 20% of the population in Canada aged at least 15 years reported having used marijuana in the previous 3 months compared with 14% of the population before marijuana legalization . In the United States, the percentage of all adults reporting marijuana use within the previous year rose from 6.7% in 2005 to 12.9% in 2015 .
Marijuana is consumed via multiple routes, including smoking, vaporizing, and eating, with inhaled methods being the most common . It may be smoked by itself or mixed with tobacco. It is usually smoked without a filter, and users inhale larger volumes with a longer breath hold compared with tobacco smokers . For measures of airflow obstruction, one marijuana joint can produce an effect similar to that of 2.5–5.0 tobacco cigarettes. Marijuana smoke contains known carcinogens and other chemicals associated with respiratory diseases.
Numerous studies have focused on the relationship of marijuana to pulmonary function tests, symptoms, and lung cancer. Two recent systematic reviews determined that heavy marijuana use can lead to respiratory symptoms similar to those in tobacco smokers, including cough, sputum production, and wheeze. The relationship of marijuana use to pulmonary function test results and lung cancer occurrence is described as equivocal, and both review studies comment on the possibility of the bronchodilatory effect of chronic marijuana smoking leading to a long-term increase in forced vital capacity.
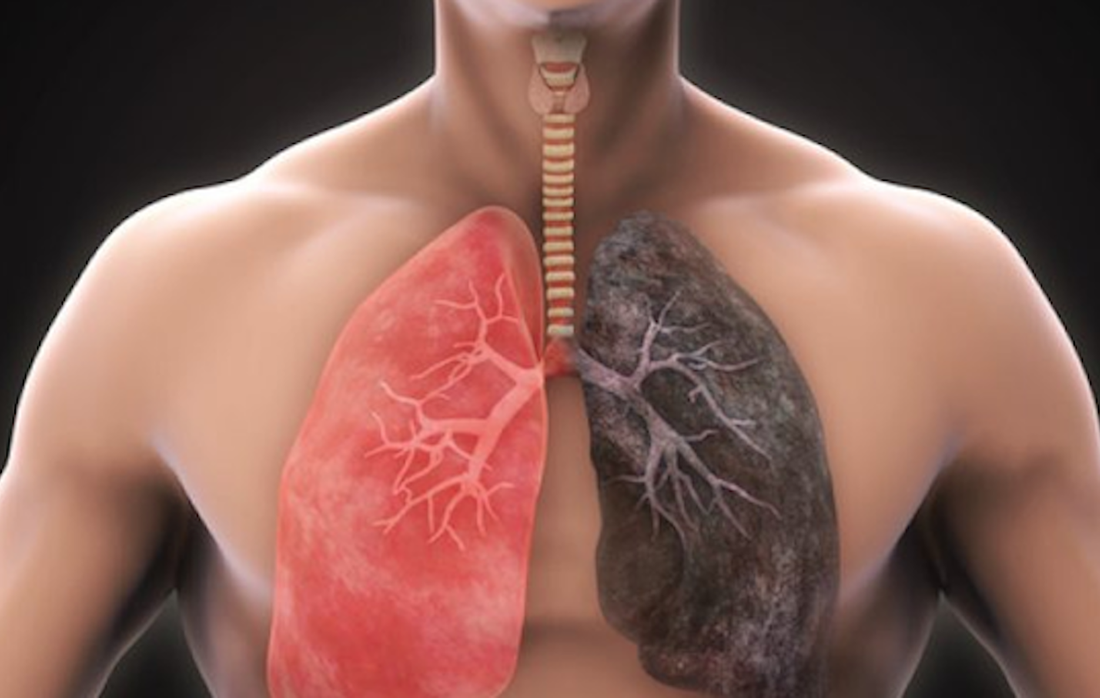
Airway inflammation and emphysema are more common in marijuana smokers than cigarette smokers, according to a new study
To find out more, Dr. Revah and colleagues compared chest CT results from 56 marijuana smokers with those of 57 non-smoking controls and 33 tobacco-only smokers.
Three-quarters of the marijuana smokers had emphysema, a lung disease that causes difficulty with breathing, compared with 67% of the tobacco-only smokers. Only 5% of the non-smokers had emphysema. Paraseptal emphysema, which damages the tiny ducts that connect to the air sacs in the lungs, was the predominant emphysema subtype in marijuana smokers compared to the tobacco-only group.
Airway inflammation was also more common in marijuana smokers than non-smokers and tobacco-only smokers, as was gynecomastia, enlarged male breast tissue due to a hormone imbalance. Gynecomastia was found in 38% of the marijuana smokers, compared with 11% of the tobacco-only smokers and 16% of the controls.
The researchers found similar results among age-matched subgroups, where the rates of emphysema and airway inflammation were again higher in the marijuana smokers than the tobacco-only smokers.
There was no difference in coronary artery calcification between age-matched marijuana and tobacco-only groups.
The results were surprising, especially considering that the patients in the tobacco-only group had an extensive smoking history.
The fact that our marijuana smokers, some of whom also smoked tobacco, had additional findings of airway inflammation/chronic bronchitis suggests that marijuana has additional synergistic effects on the lungs above tobacco. In addition, the results were still significant when they compared the non-age-matched groups, including younger patients who smoked marijuana and who presumably had less lifetime exposure to cigarette smoke.
It has been suggested that smoking a marijuana joint deposits four times more particulates in the lung than an average tobacco cigarette, irritating the airway epithelium.
The higher incidence of emphysema may also be due to the way that marijuana is smoked. Full inhalation with a sustained Valsalva maneuver, an attempt at exhalation against a closed airway, may lead to trauma and peripheral airspace changes.
SOURCE:
Luke Murtha, Paul Sathiadoss, Jean-Paul Salameh, Matthew D. F. Mcinnes, Giselle Revah (November 15, 2022). Chest CT Findings in Marijuana Smokers. Radiology. Retrieved from : https://pubs.rsna.org/doi/10.1148/radiol.212611
IMAGE:
https://www.elglaw.com/uploads/intersitial29.png