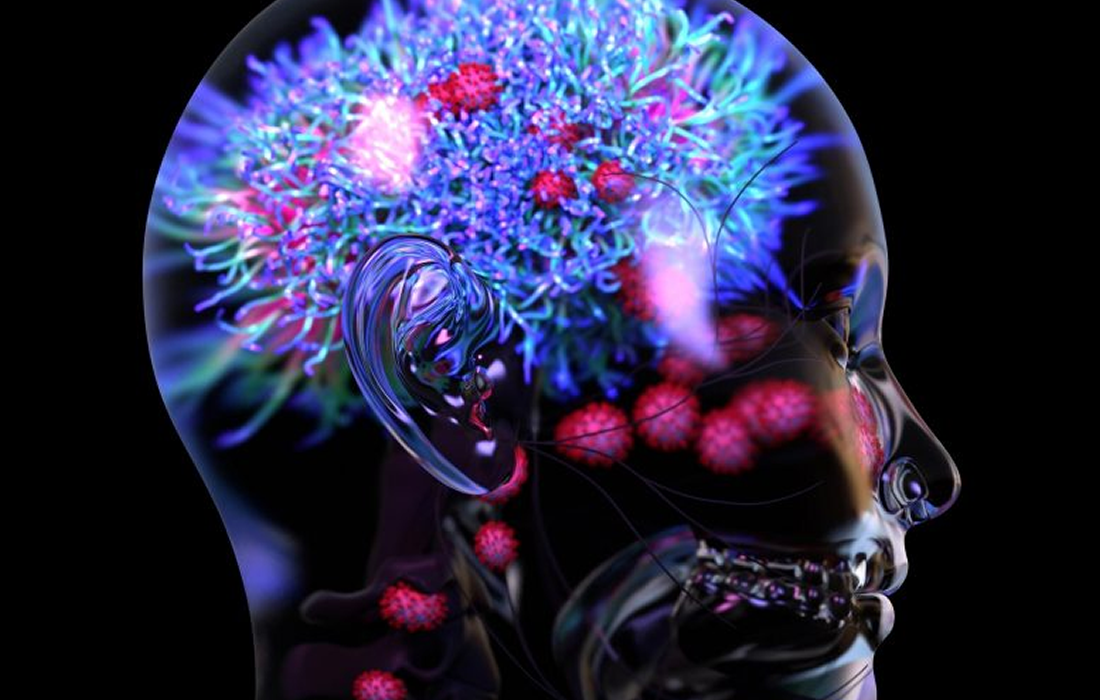
COVID-19
Cognitive Impairment Can Last Months After COVID-19 Infection
People who have survived COVID-19 frequently complain of cognitive dysfunction, which has been described as brain fog. The prevalence of post-COVID-19 cognitive impairment and the association with disease severity are not well characterized.
The COVID pandemic has now claimed as many American lives as World War I, the Vietnam War, and the Korean War combined. Most of these deaths are due to the well-known pulmonary complications of the coronavirus. It has become increasingly recognized that the virus also attacks the nervous system.
A study from the Chicago medical center found that more than 40% of patients with COVID showed neurologic manifestations at the outset, and more than 30% of those had impaired cognition.
How COVID Damages the Brain
COVID can cause damage to the brain directly by encephalitis, which may have devastating or subtle consequences.
Autopsy data from COVID patients in Finland suggests that another major cause of brain damage is lack of oxygen. Particularly worrisome is that several of the patients who were autopsied did not show any signs of brain injury during the course of their COVID infection, yet all had brain damage.
New Research Study
A new study published in the journal JAMA Network Open by Jaqueline H. Becker and colleagues analyzed data from April 2020 through May 2021 from a cohort of patients with COVID-19 followed up through a Mount Sinai Health System registry. The study involved 740 individuals, 63% (464) were women, and the mean time from COVID-19 diagnosis was 7.6 months.
The study researchers gave the participants a score for each of the assessed categories. They recorded cognitive impairment in any category in which the person scored more than 1.5 standard deviations below the expected norm for their age, educational level and sex.
On their assessment, 24% of the participants had problems with learning new information, known as memory encoding. Memory recall, which refers to retrieving previously learned information was affected in 23% of the participants and the time taken to complete a mental task, or the processing speed was slower in 18% of the participants.
They found that individuals who were admitted to the hospital had more significant effects compared to those who received treatment as outpatients or in the emergency department.
Hospitalized patients were 2.8 times more likely to show attention problems and 2.3 times more likely to have issues with memory encoding. They were also 1.8 times more likely to have issues with executive functioning, which can affect other areas of cognitive function, such as memory.
Their results raise key questions regarding patients’ long-term treatment. More studies are needed to identify the risk factors and causes underlying cognitive dysfunction as well as treatment options for rehabilitation.
Sources:
Jacqueline H. Becker, PhD, et al. Assessment of Cognitive Function in Patients After COVID-19 Infection. JAMA Netw Open. 2021; 4(10):e2130645.
doi:10.1001/jamanetworkopen.2021.30645
Katharine Lang. (2021, Oct 29). Cognitive impairment can continue for many months after COVID-19. Medical News Today. Retrieved from:
https://www.medicalnewstoday.com/articles/cognitive-impairment-can-continue-for-many-months-after-covid-19
Andrew E. Budson, MD. (2021, Mar 4). The hidden long-term cognitive effects of COVID-19. Harvard Health Publishing, Harvard Medical School. Retrieved from:
https://www.health.harvard.edu/blog/the-hidden-long-term-cognitive-effects-of-covid-2020100821133
Image from: