Platelet-Rich Plasma
Could We Use PRP to Treat Infections?
An infection occurs when another organism enters your body and causes disease. The organisms that cause infections are very diverse and can include things like viruses, bacteria, fungi, and parasites. You can acquire an infection in many different ways such as directly from a person with an infection, via contaminated food or water and even through the bite of an insect.
One type of infection, wound infections caused more commonly by bacteria, grows within the damaged skin of a wound. Symptoms can include increasing pain, swelling and redness. Wound infections with multi-drug resistant strains of pathogenic microorganisms are significant global health problems. The economic loads,morbidity and mortality rates are immense and have attracted researchers to find novel methods for infection management.
Our skin has regenerative and protective capacities in addition to acting as a barrier between the body and the outer environment. Wound healing is a complex process that is mediated by molecular interactions associated with recruitment of mesenchymal cells, proliferation and regeneration of the extracellular matrix. It includes patterns of events such as coagulation, inflammation, epithelialization, granulation tissue formation and tissue remodelling.
Platelet-rich plasma (PRP) treatment is an endogenously derived therapeutic technology that has great importance in regenerative medicine due to its potential to accelerate and stimulate tissue healing.
Platelets secrete at least seven growth factors that are essential in the initiation of the healing process, including the platelet-derived growth factor (PDGF) isomers PDGFaa, PDGFab and PDGFbb; transforming growth factor (TGF)-b1, TGF-b2, vascular endothelial growth factor (VEGF), and epithelial growth factor (EGF). These factors promote rapid increases in the number of undifferentiated mesenchymal cells at the wound site during repair and healing.
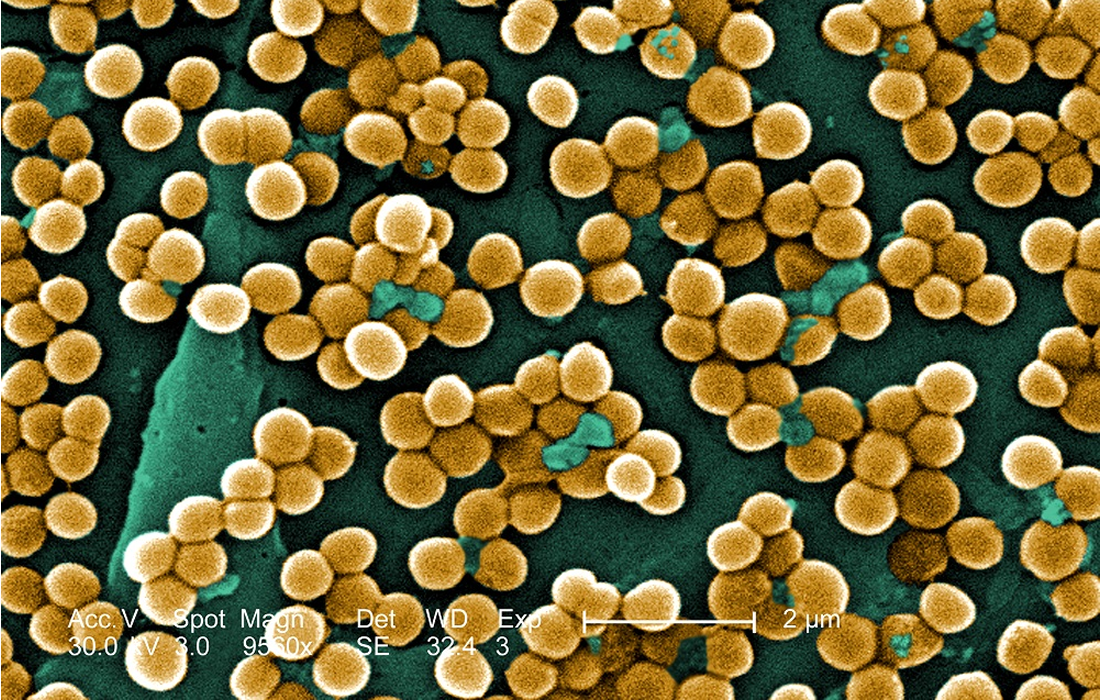
It is also believed that PRP has antimicrobial actions. Farghali et al, a group of researchers studied the antimicrobial ability of PRP in animals with methicillin-resistant Staphylococcus aureus (MRSA) wound infections. MRSA is a type of Staphylococcus resistant to methicillin and other beta lactam antibiotics, is resistant to amoxicillin, oxacillin, penicillin and many other commonly used antibiotics. It’s a major cause of hospital acquired infections in surgical wounds and even pneumonias.
They divided the study into 2 groups. One of them was treated with a regular antibiotic (clindamycin) and the other group with PRP. They evaluated the decrease in size per day of the wounds, the contraction and percentage of epithelization at 7, 15 and 21 days. They also took skin biopsies from the edges of each wound. They found a significant size reduction, wound contraction after the first week of treatment with PRP, also the re-epithelization rate was significantly increased in the PRP group at week 2. The bacterial count from the biopsies also decreased more in the PRP group compared to the control group.
They also found that proinflammatory markers like TNF-α significantly decreased in the PRP group and that the expression of the vascular endothelial growth factor (VEGF) gene was significantly higher in the PRP group. This factor stimulates wound healing via multiple mechanisms including collagen deposition, angiogenesis and epithelization.
They concluded that PRP accelerates the healing of infected skin wounds because of its antibacterial activities and rapidly reduced inflammation. These findings could potentially lead to another alternative for the treatment of difficult infections, in this case wound infections, not only as an alternative treatment but as a main therapy due to its antimicrobial, regenerative characteristics and lack of adverse effects.
Source:
Farghali, H.A., AbdElKader, N.A., AbuBakr, H.O. et al. Antimicrobial action of autologous platelet-rich plasma on MRSA-infected skin wounds in dogs. Sci Rep 9, 12722 (2019).
Source link: https://www.nature.com/articles/s41598-019-48657-5#citeas
Images from: Jain, Dr. Nikil & Gulati, Minkle. (2016). Platelet-rich plasma: A healing virtuoso. Blood Research. 51. 3-5. 10.5045/br.2016.51.1.3.