Regenerative Medicine News and General Information
Gut Bacteria Influence Brain Development
The incidence of premature birth has been rising worldwide and is one of the leading causes of perinatal morbidity and mortality. Although recent advances in neonatal intensive care have increased the survival of extremely premature infants (gestational age < 28 weeks), the number of survivors with severe morbidity and life-long neurodevelopmental impairment remains high.
The third trimester of pregnancy is a critical period for the establishment, refinement and maturation of human brain connectivity, which determines subsequent cognitive potential. Extremely premature infants are born on the verge of the third trimester and their neural circuitry is therefore established in the face of manifold environmental cues and insults associated with preterm extra-uterine life.
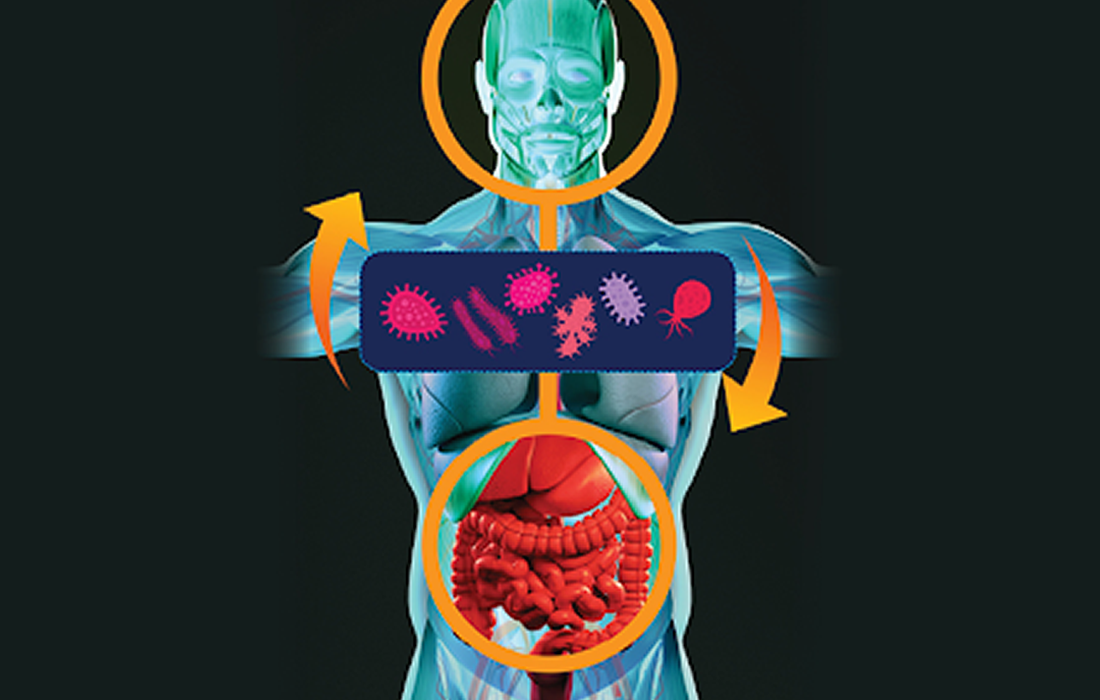
One inevitable environmental factor is the immediate postnatal colonization of the body by microorganisms. The establishing gut microbiota is in contact with a plurality of neurons of the enteric nervous system. Increasing evidence suggests that during the period of early life, enteric microorganisms participate in bidirectional signaling between the gastrointestinal tract and the brain.
Extremely premature infants are at a high risk for brain damage. Researchers have now found possible targets for the early treatment of such damage outside the brain: bacteria in the gut of premature infants may play a key role. The research team found that the overgrowth of the gastrointestinal tract with the bacterium Klebsiella is associated with an increased presence of certain immune cells and the development of neurological damage in premature babies.
Bacteria in the gut cooperate with the immune system, which in turn monitors gut microbes and develops appropriate responses to them. In addition, the gut is in contact with the brain via the vagus nerve as well as via the immune system.
The microorganisms of the gut microbiome — which is a vital collection of hundreds of species of bacteria, fungi, viruses and other microbes — are in equilibrium in healthy people. However, especially in premature babies, whose immune system and microbiome have not been able to develop fully, shifts are quite likely to occur. These shifts may result in negative effects on the brain.
The research team identified certain patterns in the microbiome and immune response that are linked to the progression and severity of brain injury. They identified that excessive growth of the bacteria Klebsiella and the associated elevated T cell levels can apparently exacerbate brain damage.
The study monitored a total of 60 premature infants born before 28 weeks gestation and weighing less than 1 kilogram for several weeks or even months. Using state-of-the-art methods the team examined the microbiome using 16S rRNA gene sequencing among other methods. The researchers analyzed blood and stool samples, brain wave recordings (e.g. aEEG) and MRI images of the infants’ brains.
The results of their study suggest that aberrant development of the gut-microbiota-immune-brain axis may drive or exacerbate brain injury in extremely premature neonates and represents a promising target for novel treatment interventions.
Source:
David Seki, et al. Aberrant gut-microbiota-immune-brain axis development in premature neonates with brain damage, Cell Host & Microbe, 2021,ISSN 1931-3128, https://doi.org/10.1016/j.chom.2021.08.004.
University of Vienna. “Gut bacteria influence brain development: Researchers discover biomarkers that indicate early brain injury in extreme premature infants.” ScienceDaily. ScienceDaily, 3 September 2021.
www.sciencedaily.com/releases/2021/09/210903132656.htm