Regenerative Medicine News and General Information
New Drug Guides Stem Cells to Desired Location
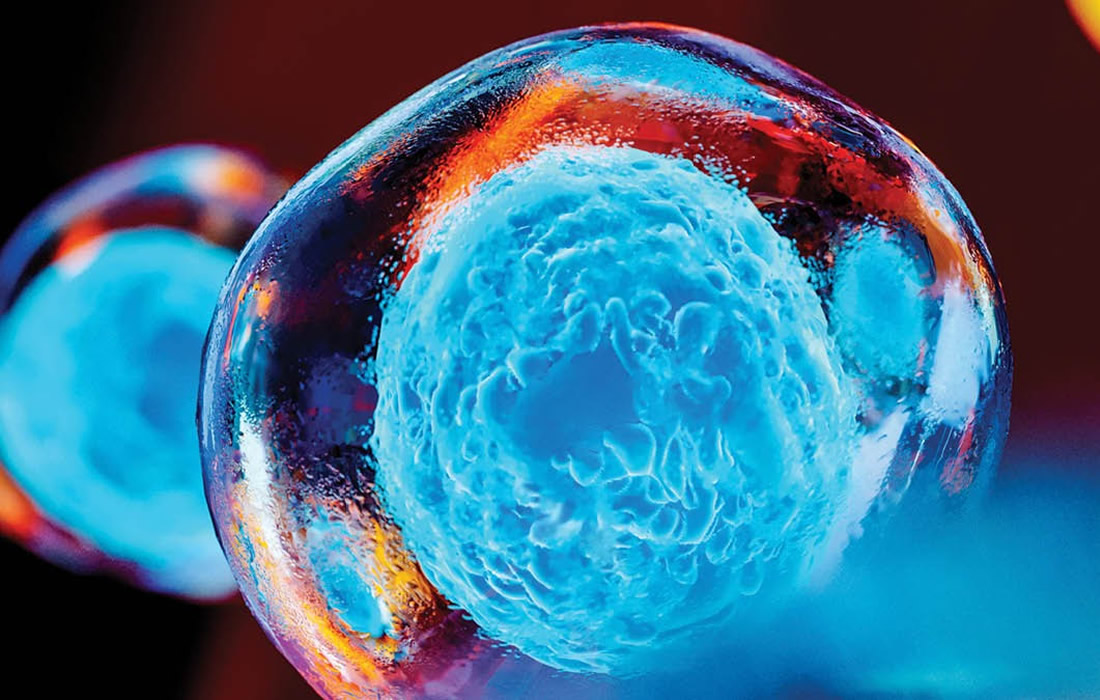
A transplanted stem cell’s engagement with a pathologic niche is the first step in its restoration of homeostasis to that site. Inflammatory chemokines are constitutively produced in such a niche; their binding to receptors on the stem cells helps direct the cell’s pathotropism (attraction of drugs or in this case cells toward diseased structures). Neural stem cells (NSCs), which express CXCR4, migrate to sites of CNS injury or degeneration in part because astrocytes and vasculature produce inflammatory chemokine CXCL12. Binding of CXCL12 to CXCR4 triggers repair processes within the NSC.
Although a tool directing NSCs to where needed has been long-sought, one would not inject this chemokine in vivo because undesirable inflammation follows their coupling.
Jean-Pyo Lee, et al. from the Sanford Burnham Prebys Medical Discovery Institute created a drug that can lure stem cells to damaged tissue and improve treatment efficacy. A major advance for the field of regenerative medicine. The discovery could improve current stem cell therapies designed to treat such neurological disorders as spinal cord injury, stroke, ALS and other neurodegenerative disorders.
Toxic cells disappeared when mice with a neurodegenerative condition received both therapeutic stem cells and the drug SDV1a- which corresponded with longer lives and delayed symptom onset. These results suggest that SDV1a can be used to improve the efficacy of stem cell treatments.
Nearly 15 years ago, Snyder and his team discovered that stem cells are drawn to inflammation, a biological “fire alarm” that signals damage has occurred. However, using inflammation as a therapeutic lure isn’t feasible because an inflammatory environment can be harmful to the body. Thus, scientists have been on the hunt for tools to help stem cells migrate to desired places in the body. This tool would be helpful for disorders in which initial inflammatory signals fade over time, such as chronic spinal cord injury or stroke and conditions where the role of inflammation is not clearly understood such as heart disease.
They created a drug called SDV1a by modifying CXCL12, an inflammatory molecule that could guide healing stem cells to sites in need of repair. This drug enhances stem cell binding, minimizes inflammatory signaling and can be injected anywhere to lure stem cells to a specific location without causing inflammation.
To demonstrate that the drug is able to improve the efficacy of stem cell treatment they implanted SDV1a and human neural stem cells into brains of mice with a neurodegenerative disease and found that SDV1a helped the human neural stem cells migrate and perform healing functions, which included extending lifespan, delaying symptom onset and preserving motor function for much longer.
The results found by the researchers may potentially benefit the field of regenerative medicine in general for the treatment, not only of neurodegenerative disorders, but also non-neurological conditions such as heart disease, arthritis and even brain cancer.
They also found that CXCL12 and its receptor are implicated in the cytokine storm that characterized COVID-19, so that could be another potential area to study.
Source:
Jean-Pyo Lee, et al. Chemical mutagenesis of a GPCR ligand: Detoxifying “inflammo-attraction” to direct therapeutic stem cell migration. Proceedings of the National Academy of Sciences, 2020; 201911444.
Sanford Burnham Prebys Medical Discovery Institute. “World’s first: Drug guides stem cells to desired location, improving their ability to heal.” ScienceDaily. ScienceDaily, 24 November
Source link: 2020.www.sciencedaily.com/releases/2020/11/201124101031.htm