Stem Cell Therapy for Specific Conditions
Stem Cell Therapy for Alzheimer’s Disease
What is Alzheimer’s Disease?
Around 50 million people live with dementia, with an estimated global cost of care being $818 billion US dollars. Dementia is a fatal clinical disorder characterized by amnesia, progressive cognitive impairment, disorientation, behavioral disturbances, and loss of normal daily function—Alzheimer’s disease is the most common type of dementia.
Most Alzheimer’s diseases are sporadic, with established risk factors such as cardiovascular disease, low education, depression, and the apolipoprotein-E4 gene.
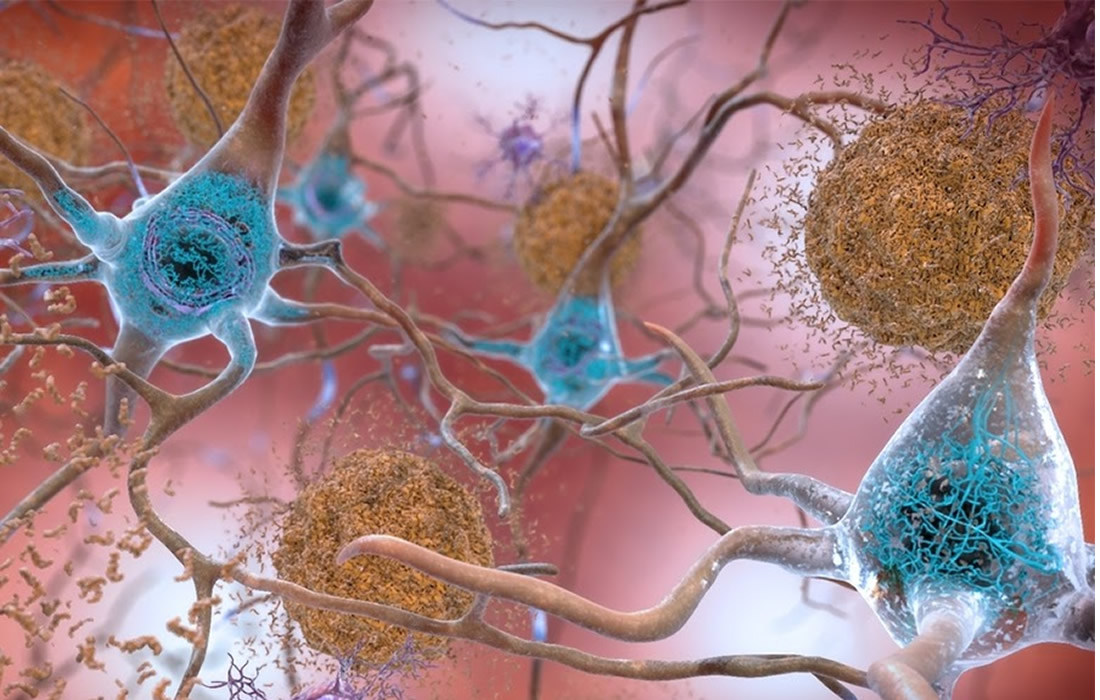
Four core features are identified in the pathology of Alzheimer’s disease:
- Neurofibrillary tangles.
- Beta-amyloid plaques.
- Activated microglia (immune cells in the central nervous system).
- Mass neuronal and synaptic loss.
Mesenchymal Stem Cells
Different studies of stem cell transplantation performed in murine models have shown modulation of inflammation and microglia immune response, anti-amyloidogenic properties, and regeneration of depleted neural networks after the administration of stem cells from different sources like human umbilical cord Wharton’s jelly-derived mesenchymal stem cell (MSC) and umbilical cord blood-derived MSC, bone marrow-derived MSC and neural stem cell.
MSCs are involved in the development of mesenchymal tissue types, which are sourced from umbilical cord blood or Wharton’s jelly. Previous studies on ucb-MSCs (mainly MSCs) using murine AD models have shown that ucb-MSCs can improve spatial learning and prevent memory decline.
Multiple mechanisms have been proposed, including reduction of Aβ plaques, BACE, and tau hyperphosphorylation, reversing microglial inflammation, and promoting anti-inflammatory cytokine.
Immunomodulatory and anti-inflammatory effects have also been observed by upregulating neuroprotection and downregulating pro-inflammatory cytokines.
This type of stem cell has been widely studied due to its accessibility and relative ease of operation. They have three prominent roles in AD treatment:
- Immune regulation.
- Reduction of Aβ plaque burden through internalization and Aβ degradation of endosomal–lysosomal pathway oligomers.
- Neurotrophic/regenerative potential.
Mesenchymal stem cells are among the most frequently studied due to their accessibility and the broad range of cell types that they can generate. In these models, their transplantation showed inhibition of Aβ related cell death, reduction of Aβ deposits and plaque formation, stimulation of neurogenesis, and neuronal differentiation.
Another therapeutic option continuously being studied is the use of MSCs derived exosomes. Exosomes are small vesicles comprised of a lipid bilayer containing various proteins, RNAs, and bioactive lipids. They act as intercellular messengers that give the ability to communicate between both cells of the same type and other cell types. Due to nanometric size (30–100 nm), MSC-exosomes reduce the possibility of vascular obstruction and cross the blood-brain barrier more easily.
Stem cell therapy for the treatment of dementia has an enormous potential that remains under development. There are a lot of studies that have demonstrated their potential therapeutic properties, but the majority of studies are in murine models. The translation between animal studies to human trials continues under investigation.
The field of cell therapy awaits the results of many ongoing clinical trials on AD. Scientists are still working to solve some of the minor technical issues in this area to pave the way for the effective treatment of AD and accelerate development.
How do we do Stem cell therapy for AD at Zignagenix?
At our clinic, we use Umbilical cord-derived Mesenchymal stem cells from Wharton’s jelly tissue. Mesenchymal stem cells have been shown in different studies a tremendous potential to modulate the immune system, decrease inflammation in various tissues, and have a paracrine effect. These results have been observed in the brains of AD patients with reduced levels of microglial inflammation and reduction of Aβ plaques, which are among the leading causes of cognitive decline in AD.
Following different research studies, one of the best ways to deliver stem cells to the brain and the affected areas in AD is by performing an intrathecal injection. At the clinic, a physician specializing in Anesthesiology with years of experience in the field will perform an intrathecal injection with mesenchymal stem cells. This way, they can travel directly from the cerebrospinal fluid to the brain and the affected areas. Also, an intravenous infusion will be performed with a high dose of mesenchymal stem cells and exosomes to boost the therapeutic effect and increase the anti-inflammatory and regenerative properties of the cells.
Source:
Tomas Duncan, Michael Valenzuela. Alzheimer’s disease, dementia, and stem cell therapy. Stem Cell Research & Therapy. 2017. 8:111.
Liu XY, Yang LP, Zhao L. Stem cell therapy for Alzheimer’s disease. World J Stem Cells. 2020;12(8):787-802. doi:10.4252/wjsc.v12.i8.787
Guo M, Yin Z, Chen F, Lei P. Mesenchymal stem cell-derived exosome: a promising alternative in the therapy of Alzheimer’s disease. Alzheimers Res Ther. 2020;12(1):109. Published 2020 Sep 14. doi:10.1186/s13195-020-00670-x