Stem Cell Therapy for Specific Conditions
Stem Cell Therapy for Antiphospholipid Syndrome
What is Antiphospholipid Syndrome?
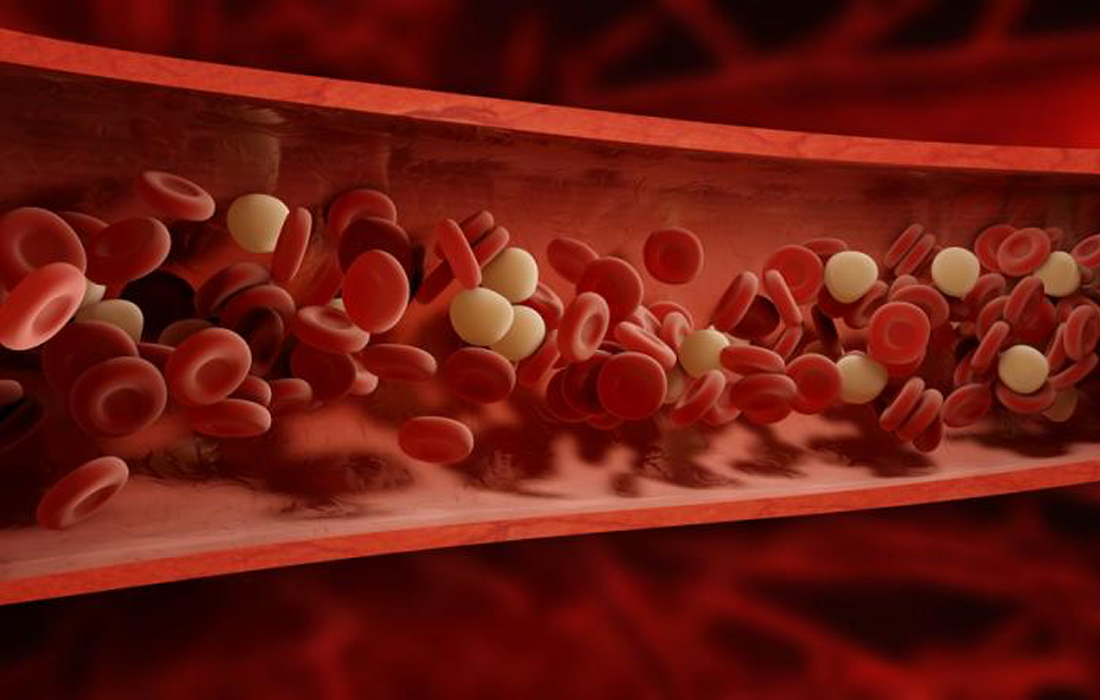
Antiphospholipid syndrome (APS) occurs when your immune system mistakenly creates antibodies that make your blood much more likely to clot. This can cause dangerous blood clots in the legs, kidneys, lungs and brain. In pregnant women, antiphospholipid syndrome also can result in miscarriage and stillbirth.
There’s no cure for antiphospholipid syndrome, but medications can reduce your risk of
Blood clots.
What Causes Antiphospholipid Syndrome?
The etiology of antiphospholipid syndrome is not completely understood. Different environmental factors have been associated to trigger the production of autoantibodies, such as infections occurring in an individual with a genetic background that makes him or her more susceptible to the disease.
Antiphospholipid antibodies (aPL) can be present in the bloodstream for a long time, but thrombotic events result only occasionally. aPL increases the risk for blood clotting, but thrombosis usually occurs when other conditions that favor clotting are present, such as prolonged inactivity, surgery or pregnancy. Other risk factors include hypertension, obesity, smoking, atherosclerosis, the use of estrogens and an associated systemic autoimmune disease, such as lupus.
What are Common Signs and Symptoms?
Signs and symptoms of antiphospholipid syndrome can include:
- Blood clots. Deep Venous Thrombosis (DVT), signs of a D.V.T include pain, swelling and redness. These clots can travel to your lungs (pulmonary embolism).
- Repeated miscarriages or stillbirths. Other complications of pregnancy include dangerously high blood pressure (preeclampsia) and premature delivery.
- Stroke. A stroke can occur in a young person who has antiphospholipid syndrome but no known risk factors for cardiovascular diseases.
- Transient ischemic attack (TIA). Similar to a stroke, a TIA usually lasts only a few minutes and causes no permanent damage.
- Rash. Some people develop a red rash with a lacy, net-like pattern.
Less common signs and symptoms include:
- Neurological symptoms. Chronic headaches, including migraines; dementia and seizures are possible when a blood clot blocks blood flow to parts of your brain.
- Cardiovascular disease. Antiphospholipid syndrome can damage heart valves.
- Bleeding. Some people have a decrease in blood cells needed for clotting. This can cause episodes of bleeding, particularly from your nose and gums. You can also bleed into your skin, which will appear as patches of small red spots.
Current Treatment Options
The conditions is often detected after a clotting event or recurrent miscarriages. Therefore, the main goal of therapy is the prevention of recurrences, because the presence of antibodies puts the patient at strong risk for future episodes.
Some lifestyle modifications and home remedies are also recommended, such as taking extra care to keep from injuring yourself and avoid bleeding when taking blood-thinning medications.
Acute thrombotic events are treated with anticoagulants (blood thinners), initially with intravenous medications, such as heparin and then followed by an oral medication like warfarin.
For pregnancy related events, heparin injections and low-dose aspirin are the standard therapy for preventing miscarriages.
Immunomodulation with glucocorticosteroids and other immunosuppressive therapies such as azathioprine, cyclophosphamide, and methotrexate could reduce the levels of aPL, especially if anticoagulants and antiplatelets have failed to prevent further thrombosis.
Stem cell transplantation has been proposed as an alternative therapeutic option for patients that are refractory to standard therapy.
Stem Cell Therapy
Studies have evaluated the use of stem cell transplantation mostly for antiphospholipid syndrome patients that also have systemic lupus erythematosus (SLE), because it is the most common disease associated with antiphospholipid syndrome.
Different studies have shown the immunomodulatory properties of mesenchymal stem cells (MSCs). They can regulate dendritic cells’ function by inhibiting their co-stimulatory molecule expression and proinflammatory cytokine production, which leads to the suppression of their capacity to initiate naive T cells and immune responses.
The studies have shown decrease in disease activity, serological features and percentage of peripheral blood regulatory T cells, which are the ones that cause the autoimmune reaction.
A systematic review published in the journal Autoimmunity Reviews included 25 studies, with a total of 279 patients with SLE and 54 of them with classification criteria of APS. The majority of the studies reported an improvement after hematopoietic stem cell transplantation in terms of disease activity control and overall survival. Some of the patients with APS even had a complete negativization of aPL after receiving the therapy and were able to discontinue anticoagulation.
Another study published in the journal Blood evaluated the use of hematopoietic stem cell transplantation (HSCT) for patients with SLE and APS. The researchers found that of the 22 patients with severe and refractory SLE with APS and chronic anticoagulation that underwent stem cell transplantation were able to discontinue anticoagulation therapy a median of 4 months after transplantation. Also, 78% of them remained free of thrombotic events and in complete SLE remission for up to 78 months.
The majority of the studies have only evaluated the use of HSCT combined with previous immunosuppression. There are studies available using umbilical cord derived stem cells (UC-MSCs) for SLE treatment but without APS.
UC-MSCs have the advantage of being able to modulate the immune system without the necessity of immunosuppression prior to the procedure and have shown good results in various studies in patients with SLE and other autoimmune conditions. More studies are needed to evaluate the use of this type of MSCs in the treatment of APS, but based on the current research studies in other autoimmune conditions and the safety shown the results seem promising.
Sources:
https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Antiphospholipid-Syndrome
Leone A, et al. Autologous hematopoietic stem cell transplantation in Systemic Lupus Erythematosus and antiphospholipid syndrome: A systematic review. Autoimmun Rev. 2017 May;16(5):469-477. doi: 10.1016/j.autrev.2017.03.008. Epub 2017 Mar 7. PMID: 28279836.
Assiri AM, Al Zahrani H, ElGohary G. Autologous Hematopoietic Stem Cell Transplantation for Antiphospholipid Syndrome: Case Report and Review of the Literature. Exp Clin Transplant. 2019 Oct;17(5):702-705. doi: 10.6002/ect.2017.0168. Epub 2018 Apr 9. PMID: 29633931.
Statkute L, et al. Antiphospholipid syndrome in patients with systemic lupus erythematosus treated by autologous hematopoietic stem cell transplantation. Blood. 2005 Oct 15;106(8):2700-9. doi: 10.1182/blood-2005-01-0330. Epub 2005 May 3. PMID: 15870182.
Image from:
https://www.medicalnewstoday.com/articles/181700