Regenerative Medicine News and General Information
Could Autism Be Related with Intestinal Inflammation?
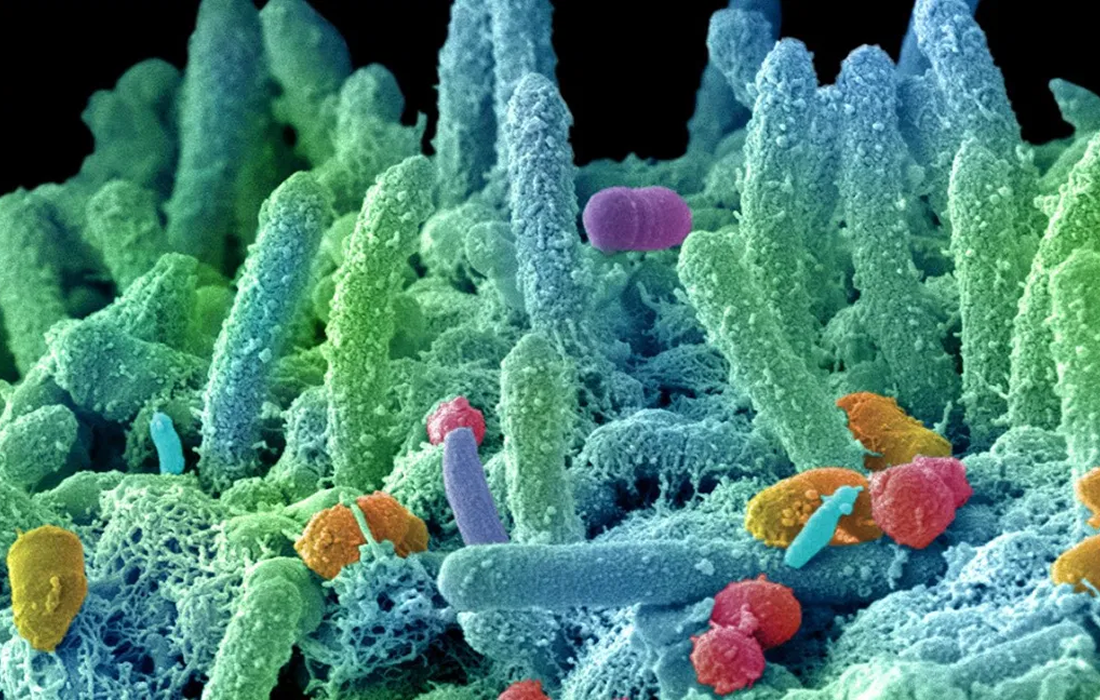
Prenatal and early life experiences are critical for human development. Studies have suggested an association between early life exposure to adverse conditions, including maternal high-fat diet, malnutrition, or infections during pregnancy with the development of different diseases, such as inflammatory and metabolic diseases as well as neurodevelopmental disorders.
Different studies have suggested that a viral infection during pregnancy correlates with an increased frequency of autism spectrum disorder (ASD) in offspring and that individuals with ASD are also known to display a broad range of non-neurological problems, including immune and gastrointestinal dysfunction.
New Study Findings
Researchers from the MIT and Harvard Medical School have recently published a study in the journal Immunity, in which they used a mouse model to investigate a connection between gastrointestinal inflammation and autism spectrum disorders.
When a mother experiences an infection during pregnancy, her immune system produces elevated levels of the molecule interleukin-17a (IL-17a), which can not only alter brain development in the fetus, but also alter her microbiome such that after birth the newborn’s immune system can become primed for future inflammatory attacks.
They used an established rodent model in which maternal immune activation (MIA) is induced in pregnant mice by injecting them intraperitoneally with the viral mimetic polyinosinic: polycytidylic acid (poly [I:C]) at embryonic day 12.5. They demonstrated that the mouse offspring exhibited autism-like phenotypes due to prenatal exposure to maternal inflammation and that they were more susceptible to developing intestinal inflammation following challenges later in life.
They also found that IL-17a generated changes in the maternal gut microbiota that led to postnatal alterations in the chromatin landscape of naive CD4+ T cells.
“We’ve shown that IL-17a acting on the fetal brain can induce autism-like behavioral phenotypes such as social deficits,” says Choi, the Mark Hyman Jr. Career Development Associate Professor in The Picower Institute for Learning and Memory and Department of Brain and Cognitive Sciences at MIT. “Now we are showing that the same IL-17a in mothers, through changes in the microbiome community, produces co-morbid symptoms such as a primed immune system.”
The researchers caution that the study findings are yet to be confirmed in humans, but that they do offer a hint that central nervous and immune system problems in individuals with autism-spectrum disorders share an environmental driver: maternal infection during pregnancy.
Sources:
David Orenstein (2021, Dec 9). Research finds potential mechanism linking autism, intestinal inflammation. MIT News. Retrieved from:
Eunha Kim, et al. Maternal gut bacteria drive intestinal inflammation in offspring with neurodevelopmental disorders by altering the chromatin landscape of CD4+ T cells. Immunity. 2021. DOI:https://doi.org/10.1016/j.immuni.2021.11.005
Image from:
https://www.healthline.com/health-news/3-ways-healthy-gut-impacts-heart-health