Stem Cell Therapy for Specific Conditions
Stem Cell Therapy for Paroxysmal Nocturnal Hemoglobinuria
What is Paroxysmal Nocturnal Hemoglobinuria?
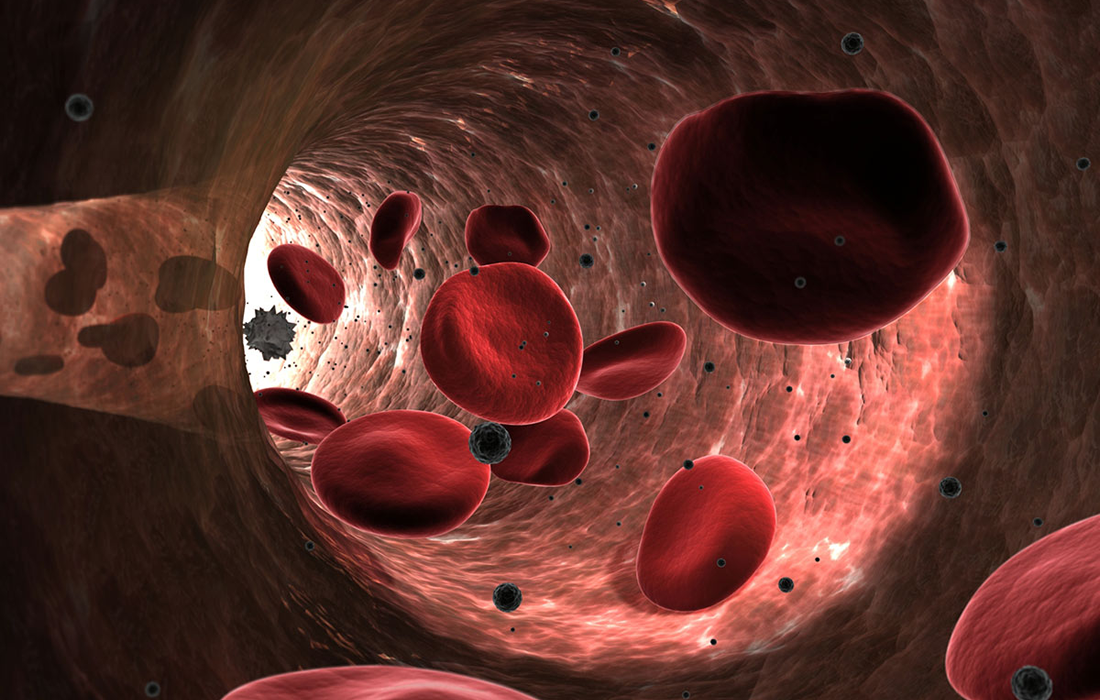
Paroxysmal nocturnal hemoglobinuria (PNH) is an acquired clonal hematopoietic cell disorder characterized by intravascular hemolysis, thrombosis and marrow failure. It is a life-threatening disease of the blood. PNH is rare with an estimated prevalence of 1 to 10 per million and has a well-defined pathophysiology in which abnormal hematopoietic cells carry mutations in the X-linked phosphatidylinositol glycal class A gene, more commonly known as PIG-A.
The median age of diagnosis is 35-40 years of age, with occasional cases diagnosed in childhood or adolescence. PNH is closely related to aplastic anemia. In fact, up to 30% of newly diagnosed cases of PNH evolve from aplastic anemia.
What Causes PNH?
Stem cells give rise to all the mature blood elements including red blood cells, which carry oxygen to our tissues, white blood cells, which fight infection, and platelets, which are involved in forming blood clots. In PNH, the affected stem cell passes the PIG-A mutation to all cells derived from the abnormal stem cell.
Cells harboring PIG-A mutations are deficient in a class of proteins called GPI-anchored proteins. Certain GPI-anchored proteins protect red blood cells from destruction, some are involved in blood clotting and others are involved in fighting infection.
The majority of PNH-related issues, including destruction of red blood cells (hemolytic anemia), blood clots (thrombosis) and infection result from a deficiency of these proteins.
What are the Common Signs and Symptoms?
Due to the wide spectrum of symptoms associated with PNH, it is not unusual for months or years to pass before the correct diagnosis is established. Overall, the most common symptoms of PNH include:
- Significant fatigue or weakness.
- Bruising or bleeding easily.
- Shortness of breath.
- Recurring infections and/or flu-like symptoms.
- Difficulty in controlling bleeding, even from very minor wounds.
- The appearance of small red dots on the skin that indicates bleeding under the skin.
- Severe headache.
- Fever due to infection.
- Blood clots (thrombosis).
Types of PNH
PNH is characterized by hemolytic anemia, bone marrow failure and a tendency toward the development of thrombosis. The condition has three main subtypes:
- Classical PNH. It includes patients who have evidence of PNH in the absence of another bone marrow failure disorder.
- PNH in the context of other primary bone marrow disorders. Such as aplastic anemia or myelodysplastic syndrome.
- Subclinical PNH. In this type of PNH, patients have small PNH clones but no clinical or laboratory evidence of hemolysis (red blood cell destruction) or thrombosis (blood clots).
Current Treatment Options
The appropriate treatment for PNH depends on the severity of symptoms. Some patients will experience few or no symptoms from PHN and do not require treatment other than folic acid and sometimes iron supplementation to increase red blood cell production. Over time, the disease may progress and more aggressive supportive care may be indicated depending on the patients’ symptoms.
The mainstay of PNH treatment is the drug eculizumab (Soliris). It is a humanized monoclonal antibody that binds to proteins in the blood that can destroy red blood cells. The drug reduces the risk of thrombosis and can improve quality of life in PNH patients. It is the only medical therapy for PNH approved by the U.S. Food and Drug Administration.
Allogeneic hematopoietic cell transplantation (HTC) remains the only cure for PNH, but eculizumab, a terminal complement inhibitor of C5, has been used to prevent complement mediated hemolysis in PNH since 2007. It does so by eliminating the defective clone and replacement with a donor hematopoietic system.
Bone marrow transplantation is not the first offered initial therapy for most patients with classical paroxysmal nocturnal hemoglobinuria given the high transplant related mortality, especially when using unrelated or mismatched donors.
The Use of Mesenchymal Stem Cells
One pilot phase I-II clinical trial studied the use of umbilical cord blood transplantation in patients that had chemoradiotherapy for acute leukemia and found that patients achieved neutrophil engraftment at a median of 19 days, platelet engraftment was 75% at a median of 53 days and patients remained alive and disease free after a follow up of 6.8 years.
Multiple studies are evaluating the use of mesenchymal stem cells for the treatment of PHN and other hematological diseases due to their immunomodulatory, support of proliferation and self renewal capabilities. The advantage of these types of cells compared with allogeneic hematopoietic cells is that they do not need to be from a matching donor and do not produce graft versus host disease.
Sources:
Cooper JP, et al. Hematopoietic Cell Transplantation for Paroxysmal Nocturnal Hemoglobinuria in the Age of Eculizumab. Biol Blood Marrow Transplant. 2019 Jul;25(7):1331-1339. doi: 10.1016/j.bbmt.2019.01.033. Epub 2019 Feb 1. PMID: 30711779; PMCID: PMC6615950.
Markiewicz M, et al. Allogeneic Hematopoietic Stem Cell Transplantation for Paroxysmal Nocturnal Hemoglobinuria: Multicenter Analysis by the Polish Adult Leukemia Group. Biol Blood Marrow Transplant. 2020 Oct;26(10):1833-1839. doi: 10.1016/j.bbmt.2020.05.024. Epub 2020 Jun 6. PMID: 32512214.
Image from:
https://www.science.org/content/article/turning-red-blood-cells-cargo-ships