Regenerative Medicine News and General Information
New Material as a Promising Treatment of Spinal Cord Injury
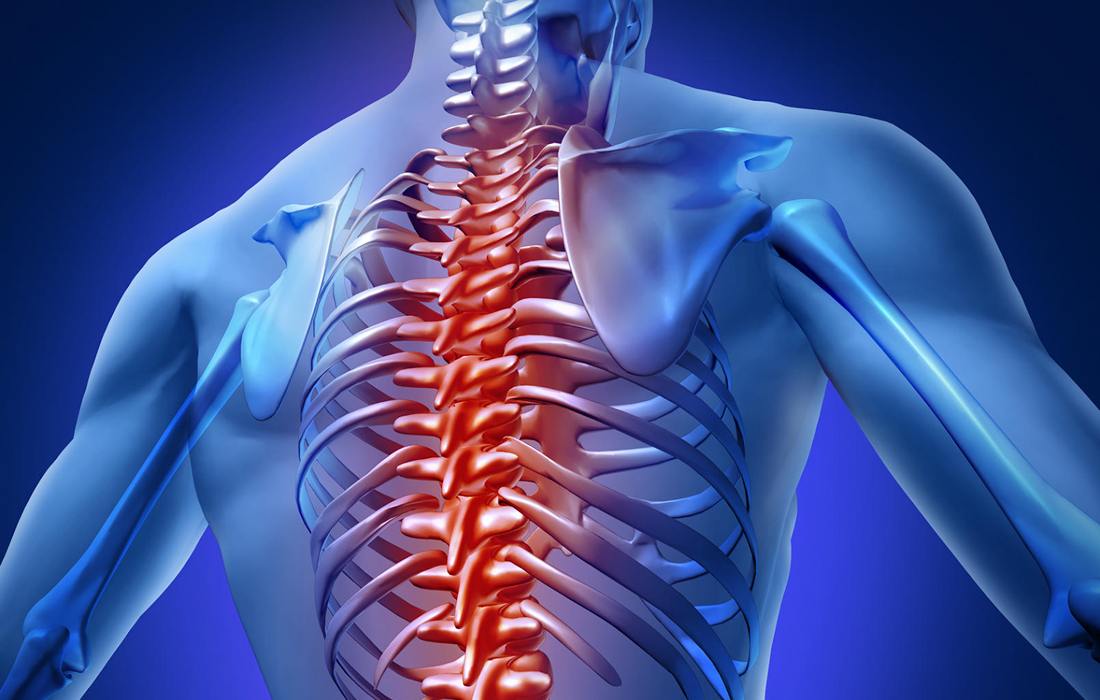
Spinal cord injury (SCI) is a traumatic event which often results in the loss of sensory and motor function, at or below the site of injury. About 12,000 new cases of SCI are reported every year in the United States alone, but due to the present clinical inability to successfully treat SCI, the amount of people suffering from this ailment is ever increasing.
Initial SCI is followed by a cascade of events, including tissue necrosis, hemorrhage, oedema, and lesion formation around the injury site. Upregulation of reactive astrocytes by means of upregulated expression of glial fibrillary acidic protein (GFAP) is one of the primary inflammatory factors. Microglia, macrophages and oligodendrocyte precursor cells aid in the formation of glial scarring around the lesion site. Still, there is much scientific debate on the influence of the glial scar on SCI regeneration. The inability of the central nervous system (CNS) cells to regenerate functional capabilities across the lesion site due to the hostile environment following injury is still a problem of major importance in SCI repair.
Unique new material has shown significant promise in the treatment of spinal cord injury
The UL team led by Professor Maurice N Collins, Associate Professor, School of Engineering at UL and lead author Aleksandra Serafin, a PhD candidate at UL, used a new kind of scaffolding material and a unique new electrically conducting polymer composite to promote new tissue growth and generation that could advance the treatment of spinal cord injury.
The research team describe a growing interest in the use of electroconductive tissue engineered scaffolds that has emerged due to the improved cell growth and proliferation when cells are exposed to a conductive scaffold.
Novel PEDOT nanoparticles (NPs) were developed in the study to overcome this limitation. Synthesis of conductive PEDOT NPs allows for the tailored modification of the surface of the NPs to achieve desired cell response and increasing the variability of which hydrogel components can be incorporated, without the required presence of PSS for water solubility.
In this work, hybrid biomaterials composed of gelatin and immunomodulatory hyaluronic acid, a material which Professor Collins has developed over many years at UL, was combined with the developed novel PEDOT NPs to create biocompatible electroconductive scaffolds for targeted spinal cord injury repair.
Biological response to the developed PEDOT NP scaffolds were studied with stem cells in-vitro and in animal models of spinal cord injury in-vivo. Excellent stem cell attachment and growth on the scaffolds was observed, they reported.
Testing showed greater axonal cell migration towards the site of spinal cord injury, into which the PEDOT NP scaffold was implanted, as well as lower levels of scarring and inflammation than in the injury model which had no scaffold, according to the study.
Overall, these results show the potential of these materials for spinal cord repair, say the research team.
Treating spinal injuries will therefore not only allow for the patient to walk or move again but will allow them to live their lives to their full potential, which makes projects such as this one so vital to the research and medical communities.
SOURCE:
Aleksandra Serafin, Mario Culebras Rubio, Marta Carsi, Pilar Ortiz-Serna, Maria J. Sanchis, Atul K. Garg, J. Miguel Oliveira, Jacob Koffler, Maurice N. Collins (November 22, 2022). Electroconductive PEDOT nanoparticle integrated scaffolds for spinal cord tissue repair. Biomaterials Research. Retrieved: https://biomaterialsres.biomedcentral.com/articles/10.1186/s40824-022-00310-5