Regenerative Medicine News and General Information
New Research on How Cancer Spreads
A study discovered a new relationship between cancer cells and the immune system, and shows how cancer can selfishly hijack a normally helpful immune pathway.
Usually, activation of this key immune pathway — called the STING pathway — triggers a strong inflammatory response that protects the body from foreign and unhealthy cells. But prolonged activation of the same pathway leads to a desensitization and ultimately to a “rewiring” of cellular signaling, which aids and abets cancer’s spread, the researchers found.
The team’s discoveries were made possible through the development of an innovative computational tool. Dubbed ContactTracing, the approach predicts cell-to-cell interactions and also examines how different cells respond to stimuli in growing tumors. By mapping interactions into a mandala-like pattern, the tool revealed that the long-term activation of the STING pathway leads to changes in cellular signaling that attracts cells that suppress the immune response to the area in and around the tumor.
Central to the research is a phenomenon known as chromosomal instability.
If the chromosomes are the instruction manual for the body, it’s like having some cells that wind up with a lot of duplicated and/or missing pages, he explains.
“We knew that chromosomal instability is an important driver of cancer’s ability to spread, otherwise known as metastasis,” Dr. Bakhoum says. “What we discovered here is that the immune system plays a central role in this process.”
A previous collaboration between researchers at MSK and Weill Cornell Medicine, showed the complex chain of events triggered by chromosomal instability leads to changes in cells that drive cancer metastasis.
To figure out the immune system’s role, the new study used mouse models of cancer that either had fully functional immune systems or greatly weakened immune systems. It also looked at tumor cells with both high and low levels of chromosomal instability, as well as cells missing the STING1 gene, which makes a protein called STING, that activates an inflammatory response when it detects foreign DNA molecules in the cytoplasm.
“What we found was that the effect was largely dependent on the immune system,” Dr. Bakhoum says. “Basically, there is sinister cooperation between cancer cells with chromosomal instability and immune cells — and that cooperation is driven by STING.”
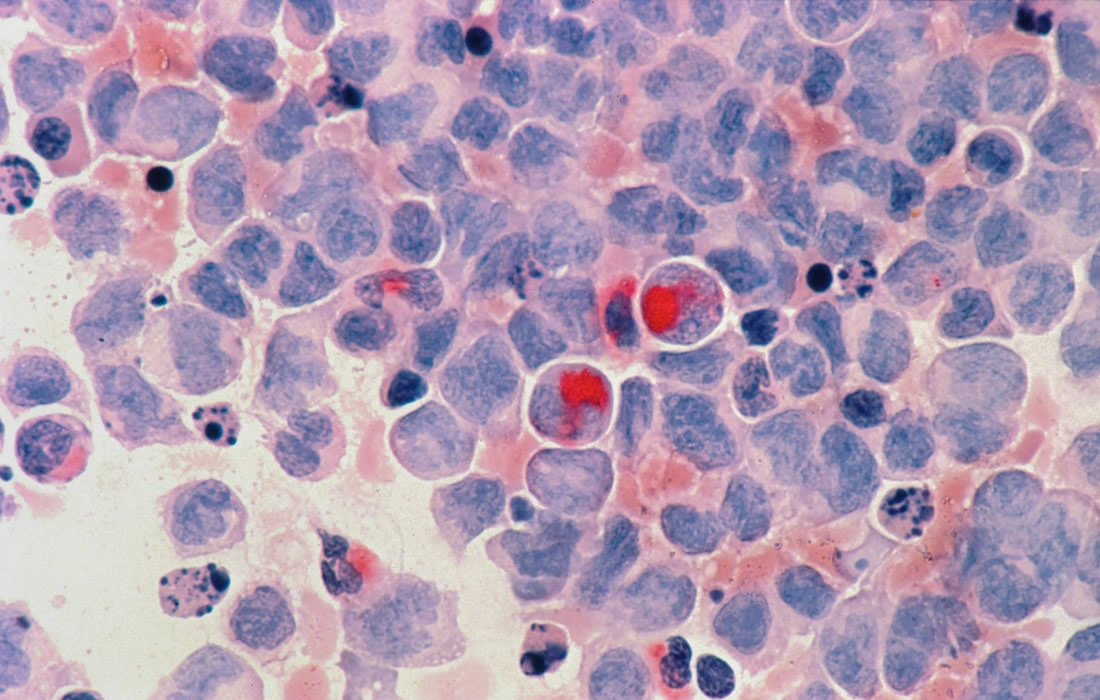
The scientists used a technique called single-cell sequencing to understand all the different cellular players in and around a tumor (also called the tumor microenvironment). The technique allows for the detailed analysis of all the many types of cells involved — such as macrophages, T cells, B cells, neutrophils, and tumor cells — and the ligands and receptors they express. Notably, to communicate, cells typically emit ligands that bind to complementary receptors on the surface of target cells, thereby triggering a change in the behavior of the target cell. While most methods predict cell-to-cell interactions based on just the mutual expression of complementary ligand-receptor pairs, the research team focused on whether their interaction actually changes the cell receiving the signal.
“One of our most important findings was that altering the level of chromosomal instability or the activation of STING dramatically changes responses in the environment in and around the tumor,” Dr. Laughney says.
And to understand those impactful interactions between the cancer cells and different immune cells, the researchers developed ContactTracing. By design, the tool exploits the variability of real-world biology without the need for prior knowledge.
The method is based on the simple premise that in a given tumor, there is inherent biological diversity — not every cancer cell is going to secrete the same binding molecule, or ligand. And not every immune cell is going to express the right receptor for that ligand, Dr. Laughney explains.
So, by comparing cells that are interacting to ones that aren’t, the tool gives scientists a clearer picture of what exactly is changed by the interaction between the two.
“When you look at the effects that elicit a response in the cancer microenvironment, all the ligands on those chromosomally unstable cancer cells were associated with a specific cellular stress response — one that happens to involve STING,” she says.
And when the same interactions were examined in the context of low chromosomal instability or where STING had been depleted from cancer cells, they trigger a different response — a strong immune response that attacks the cancer cells.
The findings from the study suggest an opportunity to improve treatments for the many patients with advanced cancer driven by chromosomal instability, Dr. Bakhoum says.
“It appears the reason activating STING in these patients isn’t very effective is that most patients’ cells are already desensitized to it due to the persistent activation of the pathway from chromosomal instability,” he says. “Counterintuitively, these patients may actually benefit from STING inhibition.”
Sources:
Jun Li, Melissa J. Hubisz, Ethan M. Earlie, Mercedes A. Duran, Christy Hong, Austin A. Varela, Emanuele Lettera, Matthew Deyell, Bernardo Tavora, Jonathan J. Havel, Su M. Phyu, Amit Dipak Amin, Karolina Budre, Erina Kamiya, Julie-Ann Cavallo, Christopher Garris, Simon Powell, Jorge S. Reis-Filho, Hannah Wen, Sarah Bettigole, Atif J. Khan, Benjamin Izar, Eileen E. Parkes, Ashley M. Laughney, Samuel F. Bakhoum. Non-cell-autonomous cancer progression from chromosomal instability. Nature, 2023; DOI: 10.1038/s41586-023-06464-z
Memorial Sloan Kettering Cancer Center. “New research shows how cancer rewires a key immune pathway to spread.” ScienceDaily. ScienceDaily, 23 August 2023. <www.sciencedaily.com/releases/2023/08/230823122523.htm>.
Images from:
Photo by National Cancer Institute
https://unsplash.com/photos/mbL91Lg56zc