Regenerative Medicine News and General Information
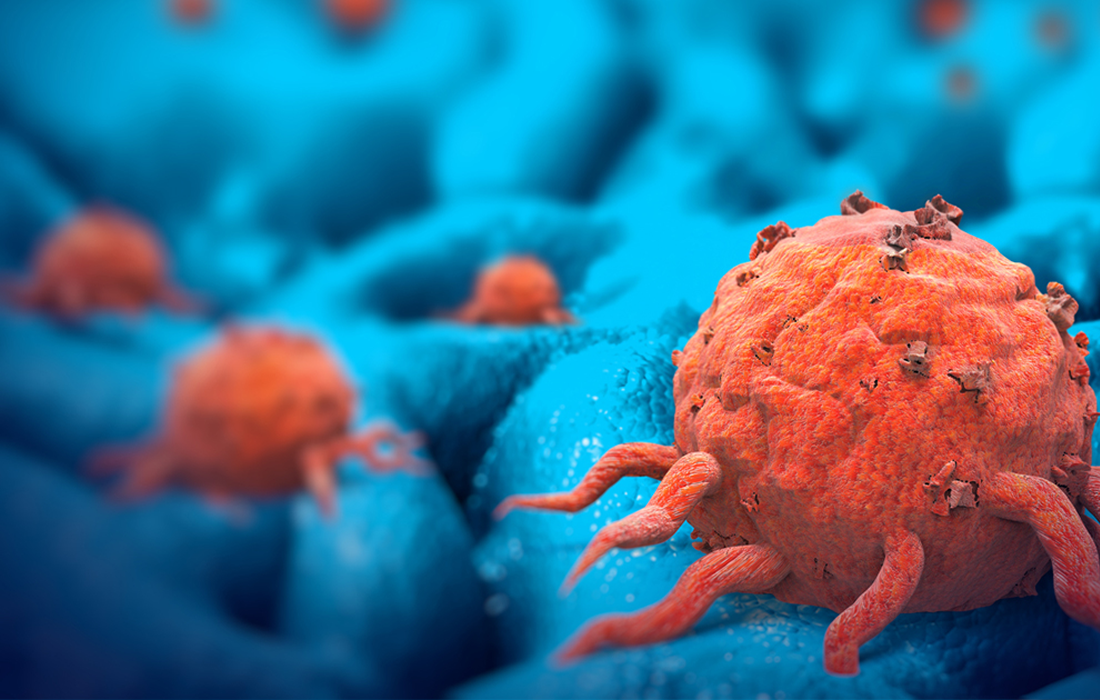
How Tumors Evade Therapy
Understanding how resistance to chemotherapy occurs could lead to better anticancer treatments. Persister cells in tumors can contribute to this resistance.
Cancer can recur when a subset of tumor cells called persister cells survive chemotherapy. Most of these cells are non-dividing (quiescent) in the presence of therapeutic drugs, but a rare subpopulation can re-enter the cell cycle during treatment which enables them to proliferate.
Persister cells are a small population of cancer cells that basically stops growing in the presence of anti-cancer drugs. Since they are not growing, chemotherapeutic agents do not attack these cells. However, once the patient is no longer taking the chemotherapeutic the dormant persisters wake up and resume growing again, which makes the complete eradication of cancer extremely difficult to achieve.
Data suggest that non-genetic mechanisms, such as changes to the complex of DNA and protein called chromatin might have a role in the development of a persistent state. Oren, et al. examined the cellular lineages and gene expression profiles of persister cells by tracing tumor cells and their descendants with a method called DNA barcoding.
DNA barcoding is a method of species identification using a short section of DNA from a specific gene or genes.
The authors analyzed cell divisions in human lung cancer cells in vitro that have a mutation in the gene encoding the epidermal growth factor receptor (EGFR). They were treated with osimertinib, an inhibitor of this receptor. They tracked the cellular lineages of the tumour cell line and found that 8% gave rise to persister cells after 14 days and 13% of the persisters resumed the cell cycle and proliferate to form colonies, which show that these type of cells arise early during the course of treatment and evolve from separate lineages.
They developed a system that they call “watermelon” to trace each cell’s lineage, proliferation status and transcriptional state. To determine if the persister state was due to a genetic, irreversible property of them, the authors re-exposed the persister cell population to osimertinib after a pause in treatment and found that cells from both cycling (dividing) and non-cycling populations reacquired drug sensitivity, suggesting that non-genetic and reversible mechanism underlies persistence.
The treatment with osimertinib induced the formation of reactive oxygen species (ROS), which can cause oxidative stress. At the end of the treatment the cycling persisters had lower levels of ROS compared to the non-cycling persisters. Also, when they decreased ROS levels in cells through the addition of ROS scavenger molecules, the fraction of persister cells that were cycling increased, suggesting that the redox state of cells has a role in the regulation of cycling persisters.
Understanding the dynamics of persister cells is crucial to the development of more effective chemotherapies for cancer treatment. The authors reported that inhibiting the pathway for fatty acid oxidation using the inhibitor drug etomoxir resulted in a decrease in fraction of cells that were persisters and the fraction of the persister that were cycling (dividing), which indicates that modulation of this pathway and genes that have functions related to it, might be worth considering in the development of new treatments.
The existence of persisters is without a doubt one of the major setbacks in cancer therapy. More studies on persister cells are needed to answer the many questions associated with them. Without a clear understanding of all the properties of persister cells, a complete treatment/eradication of cancer continues to be a complex task.
Source:
https://www.nature.com/articles/d41586-021-02117-1